Tuesday Report

From Washington, DC,
- By a 217 – 215 vote, the House of Representatives tonight passed the White House’s “big, beautiful [reconciliation] bill” — H. Con. Res. 14 — “Establishing the congressional budget for the United States Government for fiscal year 2025 and setting forth the appropriate budgetary levels for fiscal years 2026 through 2034.”
- Per a Senate news release,
- “Sen. Chuck Grassley (R-Iowa), Chairman of the Senate Judiciary Committee and a former Chairman of the Senate Finance Committee, sent a letter to UnitedHealth Group Chief Executive Officer Andrew Witty demanding detailed information on the company’s Medicare billing practices.”
- Govexec tells us,
- “The Trump administration is reshaping the top ranks of federal agencies by making more employees politically appointed and ensuring those who remain in career roles are evaluated based on how well they implement the president’s agenda.
- “The Office of Personnel Management on Monday called on all agencies to redesignate some of their Senior Executive Service employees as political appointees, rather than reserving them for career staff. On Tuesday, it announced a new performance appraisal system for career executives, which will now give the most significant weight to how well the top-level supervisors carry out the president’s policies.”
- Federal News Network informs us,
- “The Office of Personnel Management is giving an ultimatum to remote and teleworking employees who are more than 50 miles away from their official duty stations.
- “OPM is directing employees in this scenario to either report to their current duty station, agree to a “management-directed reassignment” and relocate to office space in another geographic region, or accept termination from their jobs.
- “According to presentation slides shared with Federal News Network, these are the options employees more than 50 miles of their OPM facility will receive in a “Management Direct Reassignment” memo on Wednesday.
- “OPM is giving employees until Friday, March 7 to respond.”
- and
- “Social Security beneficiaries impacted by the Windfall Elimination Provision and the Government Pension Offset may begin receiving their one-time retroactive payments as soon as this week.
- “The Social Security Administration has significantly shortened its timeline to start distributing benefit payments to public sector workers whose Social Security benefits have been impacted by WEP and GPO. SSA said it began distributing the one-time retroactive payments this week, and most payments will process incrementally over the next month.
- “The agency said in a press release Tuesday that most beneficiaries should receive their one-time retroactive payments by the end of March. The retroactive payments are backdated to January 2024.”
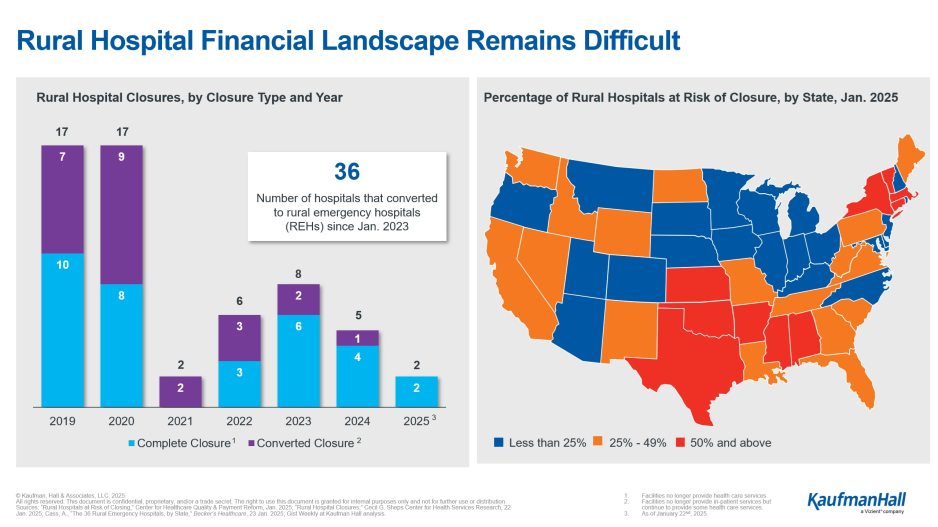
- The American Hospital Association News continues to fill us in on its rural healthcare leadership conference.
- Per Fierce Healthcare,
- “The federal government under the Trump administration has turned its focus to cutting costs, and a new report from the Blue Cross Blue Shield Association highlights policy efforts it says could save nearly $1 trillion in healthcare costs over the next decade.
- “The road map includes 10 policy proposals for stakeholders to consider, and BCBSA said these changes could drive federal savings of $524 billion, lower private insurance premiums by $389 billion and save patients $180 billion out-of-pocket.
- “The largest potential area for savings, according to the analysis, is to adopt site-neutral payments in Medicare, which the paper estimates would save $484 billion over 10 years. The report also suggests that mandating a different provider identifier for off-campus facilities than what’s required for on-campus facilities could save an additional $11 billion.”
From the judicial front,
- Fierce Pharma informs us,
- “Compounding pharmacies aren’t surrendering their ability to create cheaper knockoff versions of Eli Lilly and Novo Nordisk’s weight loss drugs without a fight.
- “In response to the FDA declaring on Friday that the shortage for Novo’s blockbuster GLP-1 treatments Ozempic, approved for diabetes and Wegovy, which has a license in obesity, was over and that compounders would have to stop producing them in the next 60 to 90 days, an organization which backs the pharmacies has filed a lawsuit (PDF) in U.S. District Court in Fort Worth, Texas.
- “The complaint alleges that the U.S. regulator is “dismissing evidence that the shortage persists,” in removing the drugs from its shortage list “without notice-and-comment rulemaking.”
- “It is the second lawsuit filed in the same court from the Outsourcing Facilities Association (OFA) and Texas-based FarmaKeio Superior Custom Compounding.
- “In October, in a complaint that is still pending, they sued the FDA after it removed Lilly’s tirzepatide—the main ingredient in its diabetes and obesity blockbusters Mounjaro and Zepbound—from its shortage list.”
From the public health and medical research front,
- Healthcare Finance reports,
- “Fewer clinicians are entering into the primary care field, and investments in primary care are on the downswing, finds a new report from the American Academy of Family Physicians and Milbank Memorial Fund.
- “According to the findings, years of neglect and chronic underinvestment by the healthcare system have left U.S. primary care in a position where it’s increasingly unable to meet patients’ needs, particularly in rural and other underserved communities.
- “The combination of worsening primary care access and sicker patients has created a cycle whereby patients use more expensive services like emergency rooms, which raises healthcare costs and premiums, further reducing affordability and access, the report said. And overall healthcare spending continues to rise faster than economic indicators, with the primary care infrastructure only receiving a small fraction of that money.” * * *
- “People are shifting away from traditional primary care providers, with about three in 10 forgoing primary care altogether between 2016 and 2022, according to FAIR Health’s 2023 analysis of private claims data.
- “That number, though, ranged from a high of 43% in Tennessee to a low of 16% in Massachusetts, suggesting significant regional variations. Of the providers who performed primary care services in that time, 56% were physicians, while 44% were nonphysicians.” * * *
- “People are increasingly turning to telehealth for their primary care needs. At 94%, the vast majority of patients are satisfied with their experience pursuing virtual primary care, and nearly four in five (79%) say it has allowed them to take charge of their health, according to a November 2022 survey released by Elevance Health.”
- Per Healio,
- “Obesity trends have stayed stable in the last couple years, whereas severe obesity has trended downward, a recently published report suggested.
- “However, the percentage of people with a healthy weight has also decreased in the decade-plus”
- “What stands out most is that younger adults experienced the greatest increase in BMI, while older adults saw a leveling off and even a decline in recent years,” Kristen Bartelt, RN, a research clinician with Epic Research, told Healio. “This shift suggests that different age groups may be experiencing unique influences when it comes to weight and health.”
- MedPage Today adds,
- “Higher adherence to the Mediterranean diet was associated with a 6% lower risk of obesity-related cancer over 15 years.
- “Risks for colorectal, liver, and kidney cancers were significantly reduced in people with medium or high adherence to the top-ranked diet.
- “Obesity-related cancer risk reduction was even greater among current and former smokers.”
- What’s more, Rheumatology Advisor notes,
- “Dietary predictors linked to reduced mortality among patients with rheumatoid arthritis included high intake of protein and fiber, along with reduced consumption of refined grains”
- “Dietary predictors linked to reduced mortality among patients with rheumatoid arthritis included high intake of protein and fiber, along with reduced consumption of refined grains”
- The NIH Research Matters bulletin covers “Boosting peanut tolerance | Artificial sense of touch | Scratching and skin inflammation”
- BioPharma Dive lets us know,
- “Ten of 11 children born profoundly deaf experienced some degree of hearing improvement after receiving an experimental gene therapy developed by Regeneron Pharmaceuticals.
- “A few of the children can now hear sound at near-normal levels, like conversational speech. One, who was 10 months old when treated and has been followed for more than a year, correctly identified spoken words, like “mommy,” “cookies” and “airplane,” without visual cues in a formal test.
- “The findings, disclosed by the company Monday alongside a presentation at a medical meeting, are a notable achievement in the development of gene therapies for congenital deafness. Other companies and groups, including Eli Lilly, France’s Sensorion and researchers at Fudan University in Shanghai, are working on similar treatments as Regeneron.”
From the U.S. healthcare business front,
- Healthcare Dive reports,
- “Health insurers wrapped up 2024 in rough shape, recording falling profits from insurance businesses and releasing guidance suggesting that medical costs could continue climbing this year.
- “In the fourth quarter, payers continued to slog through elevated medical spending in Medicare and Medicaid. Higher costs popped up in once-safe commercially insured populations, too, suggesting American workers are sicker than before.
- “All told, major publicly traded insurers’ medical loss ratios, key metrics of spending on patient care, rose an average of 2.8 percentage points from the fourth quarter of 2023 to the fourth quarter of 2024.” * * *
- “Insurers are attempting to resuscitate their profits this year, including by shedding unprofitable MA members. During fourth-quarter calls, major Medicare insurers said they’ve successfully lost members that were dragging down their margins — and shunted other beneficiaries into plan designs that give more control over spending.”
- The Wall Street Journal reports
- “Eli Lilly LLY is expanding its offerings of its hit weight-loss drug Zepbound for people who want to pay cash instead of using their health plans and reducing prices for certain dosages.
- “The pharmaceutical company said it would start selling higher dosages of its Zepbound drug, known as tirzepatide, through Lilly Direct, its direct-to-consumer business. The new dosages – in 7.5 and 10 milligram single-dose vials – will cost patients $599 per month and $699 per month, respectively.
- “The price for both dosages goes down to $499 per month if patients refill their prescriptions within 45 days, as part of a type of customer loyalty program.
- “The company also cut the per-month price of the lower dosages by about $50. The 2.5-mg vials will cost $349, down from $399; the 5-mg vials will be $499, down from $549.
- “Lilly Direct allows patients to bypass insurers and traditional pharmacies. Lilly said it had received requests from many patients to offer the higher doses.
- “We can’t wait until the complex healthcare system is offering access to anti-obesity medications like all other chronic diseases,” said Patrik Jonsson, president of Lilly’s cardiometabolic health unit. “But in the meantime, this is a response to patients’ requests.”
- Fierce Pharma adds,
- “Looking to avoid a repeat of the shortages that plagued Mounjaro and Zepbound during their initial rollouts, Eli Lilly is building supply of its oral GLP-1 contender orforglipron well before the drug’s expected approval in 2026.
- “As of Dec. 31, Lilly had amassed pre-launch inventory worth $548.1 million that was “primarily related to orforglipron,” the company said in its annual report issued last week.
- “When we believe that future commercialization is probable and the future economic benefit is expected to be realized, we capitalize prelaunch inventory prior to regulatory approval,” the company explained in its securities filing.”
- MedCity News explains why “‘The Hardest Thing Is Separating the Wheat from the Chaff’: 5 Leaders on the State of Healthcare AI. Healthcare AI is developing at a rapid rate, and the industry’s attitude on how to best regulate and deploy this technology is evolving every day, according to leaders attending this year’s ViVE conference.”
- Beckers Hospital Review discloses average physician assistant pay, by state, and seven recent hospital closures.
- Per MedTech Dive,
- “Quest Diagnostics has struck a deal to buy kidney disease laboratory testing service assets from Fresenius Medical Care, the companies said Monday.
- “The acquisition will add dialysis-related water testing to Quest’s portfolio. Quest will perform the tests and other end-stage kidney disease laboratory services for Fresenius Medical Care’s dialysis centers in the U.S.
- “Quest, which has not disclosed the value of takeover, completed eight buyouts last year, but CEO Jim Davis recently told investors the company would “moderate” its dealmaking pace in 2025.”
- and
- “Thermo Fisher Scientific agreed to pay about $4.1 billion in cash to acquire Solventum’s purification and filtration business.
- “The technologies, used in the production of biologics and medical devices and for industrial applications, generated about $1 billion in revenue last year. The business employs about 2,500 people globally and will become part of Thermo Fisher’s life sciences solutions segment.
- “The Solventum unit is highly complementary to Thermo Fisher’s bioproduction business that offers cell culture media and single-use technologies, Thermo Fisher CEO Marc Casper said in the Tuesday announcement.”