Friday Stats and More
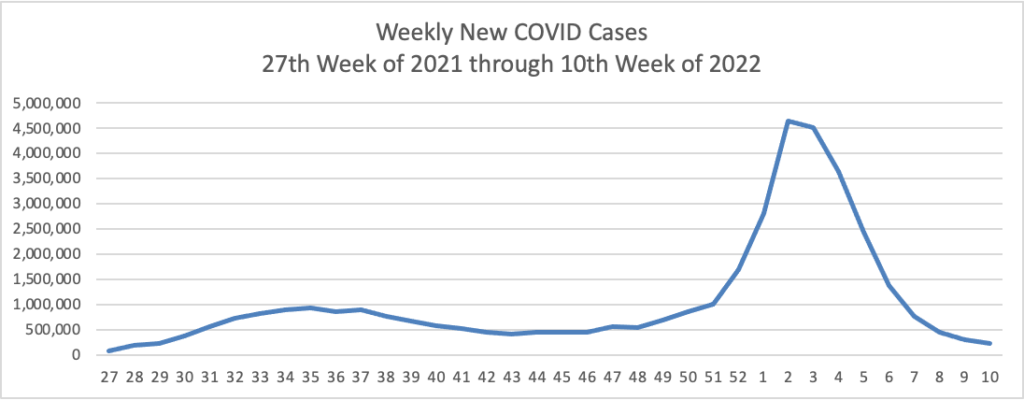
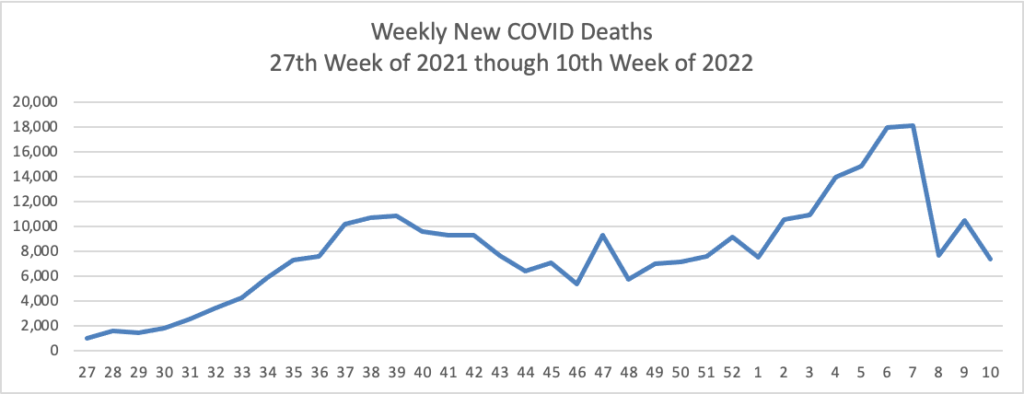
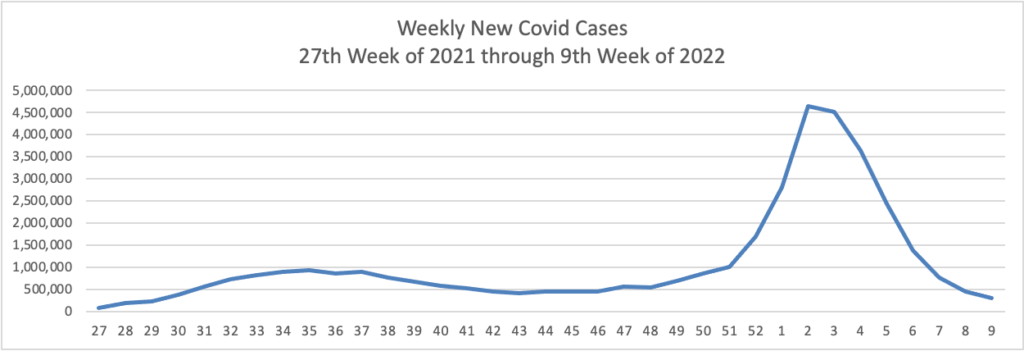
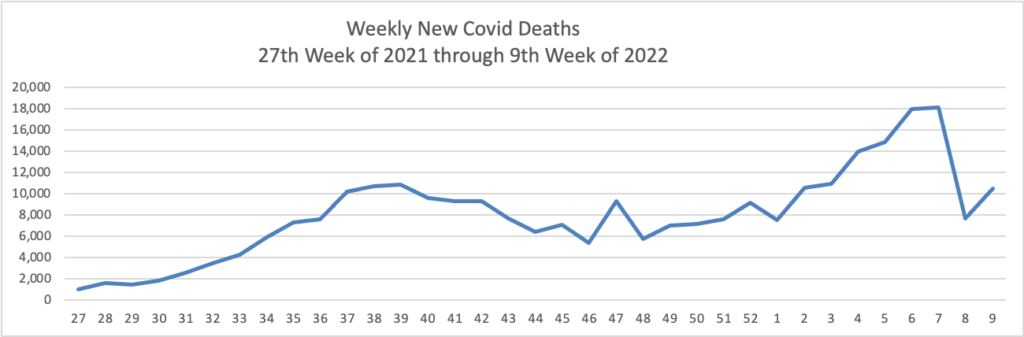
Based on the Centers for Disease Control’s Covid Data Tracker and using Thursday as the first day of the week, here is the FEHBlog’s latest weekly charts of new Covid cases and deaths (a lagging indicator):
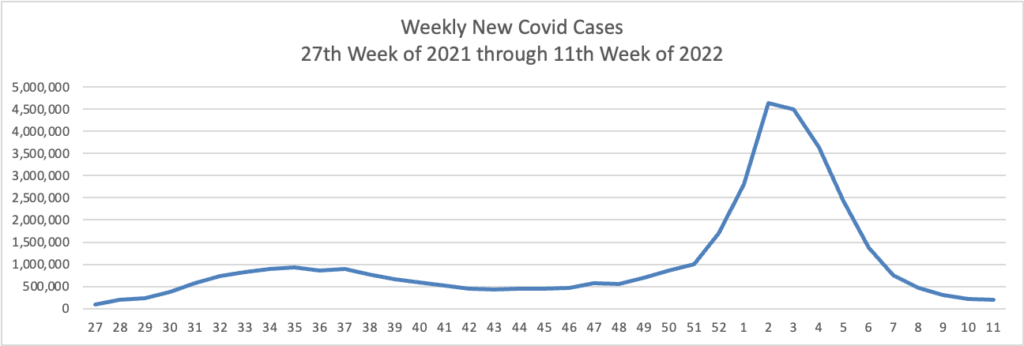
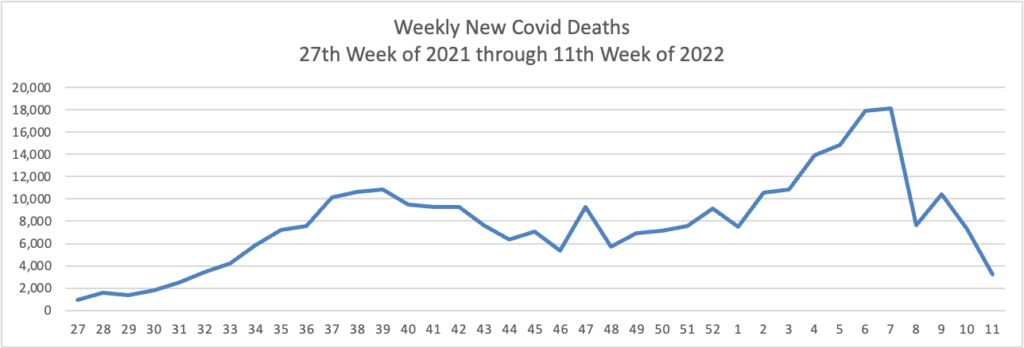
The CDC observes in its weekly review of its Covid statistics
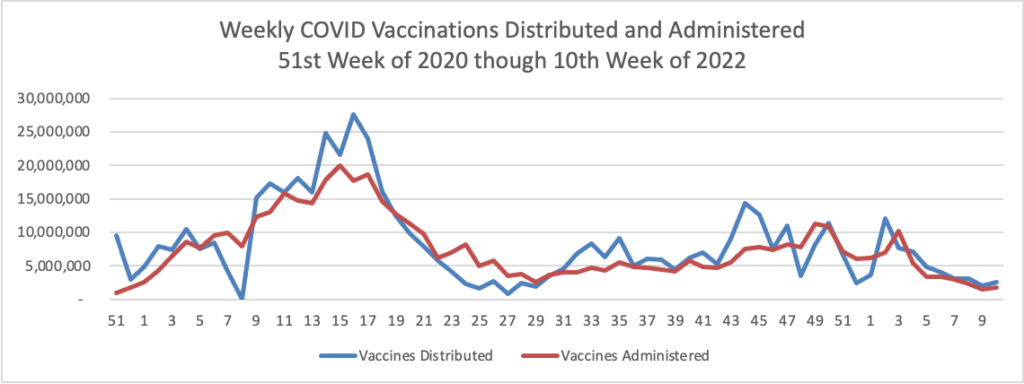
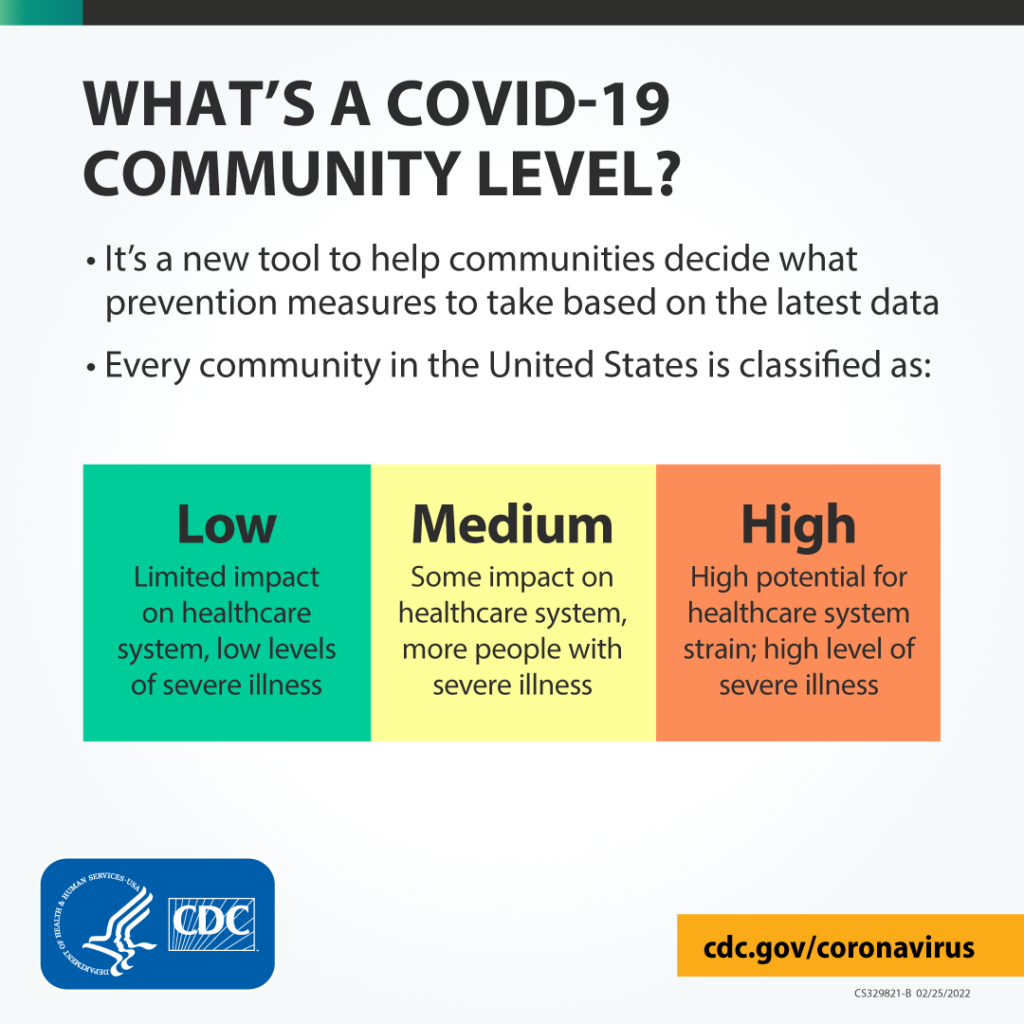
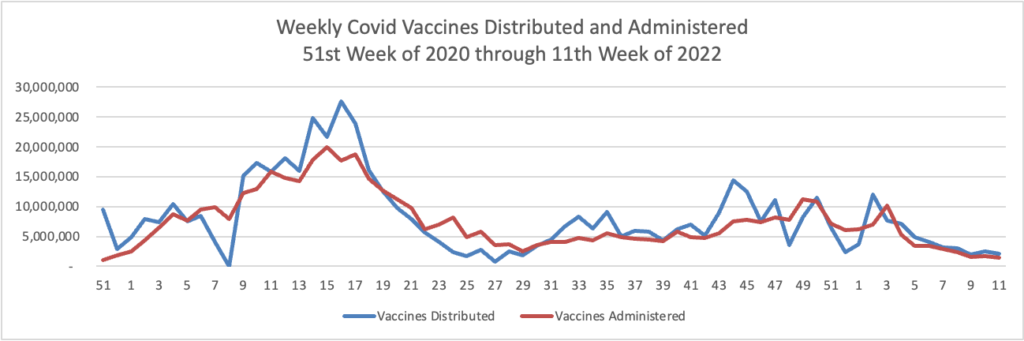
COVID-19 cases, hospitalizations, and deaths all continue to decrease in the United States. According to CDC’s COVID Data Tracker, as of March 16, 2022, 76.7% of the total U.S. population has received at least one dose of a COVID-19 vaccine, and 65.3% has completed their primary series. However, only about half of the booster-eligible population has received a booster dose and is considered up to date on their COVID-19 vaccines.
Two new studies show the effectiveness of COVID-19 vaccines and boosters across periods of three variants of concern (Alpha, Delta, and Omicron). CDC released a study today showing that, among adults hospitalized with COVID-19 during the Delta and Omicron waves, those who received two or three doses of the Pfizer-BioNTech or Moderna vaccine had 90–95% less risk of dying or needing a ventilator compared with adults who were not vaccinated. Protection was highest in adults who received a third COVID-19 vaccine dose. A study published in the British Medical Journalexternal icon found that vaccines gave a high level of protection against hospitalization for all variants, but not as much for Omicron among adults who received only a primary series. However, boosters increased protection against Omicron. The study also showed that hospital patients who were vaccinated had much lower disease severity than patients who were not vaccinated.
These studies emphasize the importance of staying up to date with vaccinations—they are our best protection against severe COVID-19 illness. Vaccination is also the safest way to reduce the chance that new variants will emerge. Find a vaccine provider and get your booster dose as soon as you can.
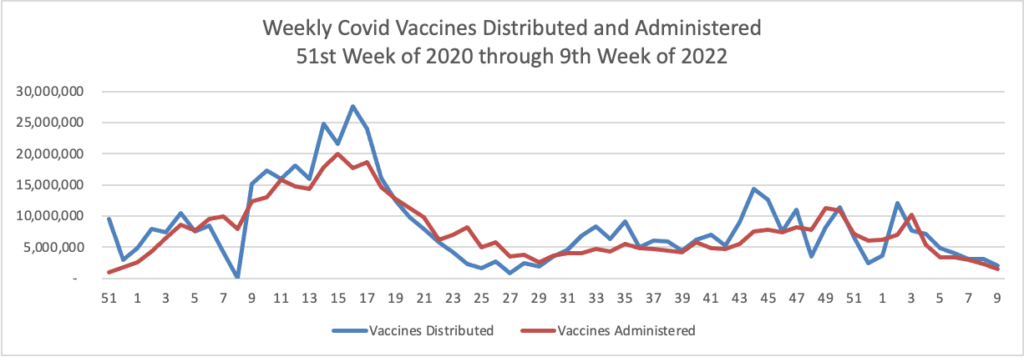
In that regard, here is the FEHBlog weekly chart of Covid vaccinations distributed and administered from the beginning of the vaccination era in late 2020:
Here’s a link to the Food and Drug Administration’s March 18 round of its Covid related activities.
While the bulk of Covid care spending goes to hospitals, Becker’s Hospital Review reports that a “sizable minority” have a significant amount out-of-pocket spending for this care, according to a study published in the American Journal of Managed Care March 16.”
It’s worth adding that the Wall Street Journal reports that
The biggest credit-reporting firms will strip tens of billions of dollars in medical debt from consumers’ credit reports, erasing a black mark that makes it harder for millions of Americans to borrow.
Equifax Inc., Experian PLC and TransUnion are making broad changes to how they report medical debt beginning this summer. The changes, which have been in the works for several months, will remove nearly 70% of medical debt in collections accounts from credit reports.
Beginning in July, the companies will remove medical debt that was paid after it was sent to collections. These debts can stick around on a consumer’s credit report for up to seven years, even if they are paid off. New unpaid medical debts won’t get added to credit reports for a full year after being sent to collections.
The firms are also planning to remove unpaid medical debts of less than $500 in the first half of next year. That threshold could rise, according to people familiar with the matter.
From the compliance front —
- The Internal Revenue Services issued a notice on how to calculate the No Surprises Act’s Qualified Payment Amount when the health plan does not have enough data to calculate a January 2019 median.
- The Department of Labor is offering a webinar on March 30 at 11 am that “will help employers, service providers, and benefit professionals understand how the provisions of [the federal mental health partity act] apply to employer-sponsored group health plans and provide information on how to avoid common problems. The webinar runs about 45 minutes to an hour and is limited to 200 participants.
From this week’s healthcare conferences front
- Fierce Healthcare discusses the electronic medical records interoperability theme of the HIMSS conference.
- Fierce Healthcare also offers a wrap report on “the most interesting innovations at SXSW 2022: From holograms to the future of psychedelics.”
From the telehealth front
- Becker’s Payer Issues reports that most consumer driven plans have taken advantage of the IRS offered flexibility to cover telehealth before the “high” annnual deductible.
- Forbes informs us “Telehealth Accounts For One In Three Mental Health Visits Two Years Into Pandemic.” Whoopee.
From the good works department, the American Medical Association tells us about a North Carolina physician who is talking the diabetes problem.
Dr. [Brian] Klausner is the medical director of WakeMed’s Community Population Health program in Raleigh. He also is a physician champion for DiabetesFreeNC. That is the statewide initiative where AMA partnered with the North Carolina Medical Society and others to support collaborative efforts to end type 2 diabetes in the Tar Heel State.
Rather than think of the pandemic as having “derailed” diabetes prevention or other population health efforts, Dr. Klausner said that “COVID-19 expedited new perspective in how we can do a better job addressing historic roadblocks to community health initiatives, including those related to diabetes and prevention.”