Tuesday Tidbits

From Washington, DC,
- The Washington Post reports,
- “Republican lawmakers returned to Capitol Hill on Tuesday with some spring in their step.
- After winning the presidency and the Senate majority, the party is on the cusp of regaining the House majority — and with it, a powerful governing trifecta in Washington.
- “Though control of the House may not be called for days, GOP lawmakers will this week work on the assumption they’ve clinched it, pushing ahead with House leadership elections and shaping plans to reverse or overhaul much of the Biden administration’s domestic and foreign policy.
- “Though control of the House may not be called for days, GOP lawmakers will this week work on the assumption they’ve clinched it, pushing ahead with House leadership elections and shaping plans to reverse or overhaul much of the Biden administration’s domestic and foreign policy.”
- The Post must be tracking the AP results (214 – 206) because Decision Desk HQ has decided that the Republicans do have a majority of seats in the House (219 – 210, 218 being a majority).
- The Wall Street Journal reports,
- “President-elect Donald Trump picked Tesla CEO Elon Musk and biotech company founder Vivek Ramaswamy, a former Republican presidential candidate, to lead an effort to cut spending, eliminate regulations and restructure federal agencies.
- “Trump said in a statement Tuesday night that Ramaswamy and Musk—the wealthiest person in the world, who oversees six companies including Tesla—would lead what the president-elect called the Department of Government Efficiency, or DOGE. The department’s mandate is to streamline government bureaucracy, the president-elect said.
- “DOGE will operate outside of the federal government, Trump said, and will work with the White House Office of Management and Budget to implement its recommendations.”
- The American Hospital Association News lets us know,
- “In comments Nov. 12 to majority and minority leaders of the House and Senate, the AHA requested that Congress act on key priorities for hospitals and health systems before the end of 2024. AHA urged Congress to continue providing relief from Medicaid Disproportionate Share Hospital Payment cuts; continue the Medicare-dependent Hospitals and Low-volume Adjustment programs that expire Dec. 31; reject site-neutral payment proposals; and pass the Improving Seniors’ Timely Access to Care Act (H.R. 8702/ S. 4532), legislation that would reduce the wide variation in prior authorization methods in the Medicare Advantage program.” * * *
- “AHA also urged Congress to extend the hospital-at-home waiver for five years through 2029; mitigate scheduled physician reimbursement cuts for 2025; and pass the Safety from Violence for Healthcare Employees Act (H.R. 2584/S. 2768), legislation that would provide federal protections from workplace violence for hospital workers, similar to protections for airport and airline workers.”
- and
- “The Centers for Medicare & Medicaid Services Nov. 12 released a report evaluating past and present approaches to rural health. It shares how previous CMS Innovation Center models focusing on rural health have been applied to recent model development.
- “The report also shares themes, concepts and next steps gathered from its rural health “Hackathon,” a series of events across the U.S. that brought experts together to brainstorm solutions to rural health challenges. The top themes highlighted a need for training, regulatory changes and collaboration to help improve access to care and support transformation. The report also outlines possible considerations for future Accountable Care Organization-focused and other models.
- “CMS’ next intention is to issue a request for application to fill the 10 open spaces for its Rural Community Hospital Demonstration. The program was directed by Congress and requires a test of cost-based payment for Medicare inpatient services for rural hospitals with fewer than 51 beds that are ineligible for critical access hospital status.”
- OPM issued a press release today about the ongoing Open Season while Govexec informs us,
- “Retired and active federal employees find selecting a health care plan to be more confusing than creating a will, reading Shakespeare, learning a new language or navigating a divorce, according to a new survey from the National Active and Retired Federal Employees Association.
- “While the process may be complex, NARFE is urging current and former federal and postal employees to look at their options for health care insurance carriers and coverage plans during this year’s open season, which lasts from Nov. 11 through Dec. 9, especially in light of premium price increases next year that will be the largest in recent memory.
- “John Hatton, NARFE’s staff vice president of policy and programs, told Government Executive that enrollees could be missing out on thousands of dollars in savings.
- “We always recommend people to take a look at their options during open season to make sure they have the coverage that they need so they’re not paying more in out-of-pocket expenses later, but also to pay less in premiums if they don’t need the coverage that they currently have,” he said.
- “More than half of active federal employees (57%) and retired ones (55%) in NARFE’s survey annually review their health insurance options. For this year’s open season, 60% of current feds responded that they are planning on participating compared to 47% of retirees.”
- RAND shares survey results about U.S. veterans’ families, which should be of interest to FEHB carriers as the federal government wisely hire a lot of veterans.
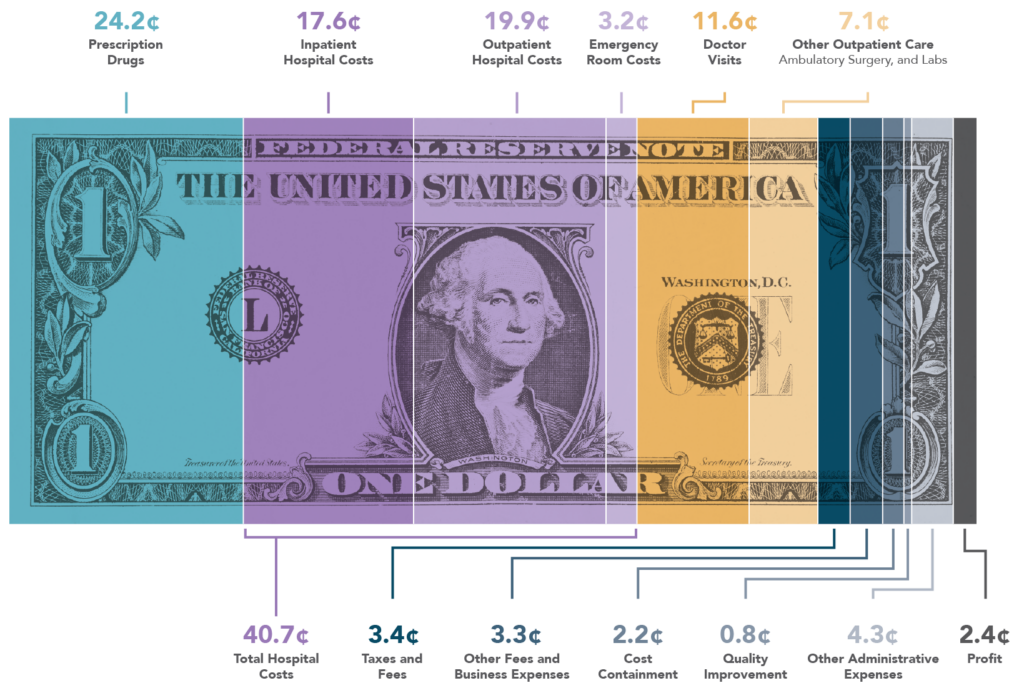
- Meanwhile, AHIP fact checks a Wall Street Journal article criticizing the Medicare Advantage program.
- The New York Times reports,
- “The Justice Department and four Democratic state attorneys general on Tuesday filed an antitrust lawsuit against the giant UnitedHealth Group in an attempt to block its $3.3 billion deal to take over Amedisys, a large home health company.
- “Unless this $3.3 billion transaction is stopped, UnitedHealth Group will further extend its grip to home health and hospice care, threatening seniors, their families and nurses,” Jonathan Kanter, the assistant attorney general who heads the department’s antitrust division, said in a statement on Tuesday.“
- The Wall Street Journal adds,
- “Johnson & Johnson launched a legal challenge against a federal health agency blocking the company’s quest to tighten the way it provides lucrative drug discounts to hospitals.
- “J&J filed a lawsuit in federal court in Washington on Tuesday against the heads of the U.S. Department of Health and Human Services and one of its agencies, seeking a court ruling that says J&J’s plan is legal and to prevent the agency from rejecting it.
- “The lawsuit escalates the pharmaceutical industry’s fight to rein in the federal drug-discount program known as 340B. The program, created in 1992, requires drugmakers to provide steep discounts on outpatient drugs to hospitals and clinics that serve uninsured and low-income patients.
- “The pharmaceutical industry has argued that the 340B program has strayed from its original purpose of helping safety-net hospitals. Manufacturers say they sell medicines to covered hospitals at steep discounts, but some large hospitals mark up the prices charged to both uninsured patients and insurers.”
From the public health and medical research front,
- The New York Times reports,
- “After decades of unrelenting increases, rates of sexually transmitted infections in the United States are showing hints of a downturn.
- “Diagnoses of gonorrhea dipped in nearly all age groups last year, compared with 2022, and new cases of syphilis and chlamydia remained about the same, according to data released on Tuesday by the Centers for Disease Control and Prevention.
- “The results are not yet cause for celebration.
- “Overall, more than 2.4 million new S.T.I.s were diagnosed last year, about a million more than the figure 20 years ago. Nearly 4,000 babies were diagnosed with congenital syphilis last year, and 279 of them were stillborn or died soon after.
- “Still, experts said they were cautiously optimistic that a resurgent tide of infections was beginning to turn.”
- Per a National Institutes of Health press release,
- “Researchers at the National Institutes of Health (NIH) and their collaborators have discovered a new way in which RAS genes, which are commonly mutated in cancer, may drive tumor growth beyond their well-known role in signaling at the cell surface. Mutant RAS, they found, helps to kick off a series of events involving the transport of specific nuclear proteins that lead to uncontrolled tumor growth, according to a study published Nov. 11, 2024, in Nature Cancer.
- “RAS genes are the second most frequently mutated genes in cancer, and mutant RAS proteins are key drivers of some of the deadliest cancers, including nearly all pancreatic cancers, half of colorectal cancers, and one-third of lung cancers. Decades of research have shown that mutant RAS proteins promote the development and growth of tumors by activating specific proteins at the cell surface, creating a constant stream of signals telling cells to grow.” * * *
- “The study also found evidence that mutant RAS proteins perform this same function in other cancer types, suggesting that this mechanism may be a general feature of cancers with mutated RAS genes.
- “The researchers believe their finding may have potential applications for the treatment of RAS-fueled cancers. They have started to look at how this function for RAS works in pancreatic cancer in particular because there are so few effective treatments for this type of cancer.
- “New treatment combinations could one day be developed that take this new role for RAS into consideration,” Dr. [Douglas] Lowy said.”
- Health Day tells us,
- “Lives lost to obesity-related heart disease have nearly tripled over the past twenty years, a new study reports.
- “Heart disease deaths linked to obesity increased 2.8-fold between 1999 and 2020, according to findings presented today at the American Heart Association’s annual meeting in Chicago.
- “The increase occurred especially among middle-aged men, Black adults, Midwesterners and rural residents, researchers found.
- “Obesity is a serious risk factor for ischemic heart disease, and this risk is going up at an alarming rate along with the increasing prevalence of obesity,” lead researcher Dr. Aleenah Mohsin, a post-doctoral research fellow at Brown University in Providence, R.I., said in a news release.” * * *
- “The National Institute of Health has more on the health risks of obesity.”
From the U.S. healthcare business front,
- Fierce Healthcare surveys the major payors’ third quarter financial results as the curtain falls on the third quarter announcement season.
- Kaufmann Hall relates,
- “Though most indicators were down, hospital performance remained relatively stable overall, according to September data. Both inpatient revenue and average lengths of stay increased.
- “The recent issue of the National Hospital Flash Report covers these and other key performance metrics.”
- and
- “In the third quarter of this year, the median investment/subsidy per physician was $304,312—rising above $300,000 for the first time. Other expense metrics such as the total direct expense per provider FTE and labor as a percentage of total expenses increased.
- “The Physician Flash Report features the most up-to-date industry trends drawn from the same data physician groups use to track their finances and operations.”
- Per Modern Healthcare,
- “Ochsner Health may expand its hospital-at-home program throughout the entire health system after successfully piloting a program in New Orleans, the nonprofit healthcare provider said Tuesday.
- “Ochsner Health said in a news release the pilot, launched in March at Ochsner Medical Center-New Orleans, prevented either initial hospitalizations or 15-day hospital readmissions for 92% of the patients referred to the program through its emergency department and observation unit.
- “The New Orleans-based health system offered the service through a partnership with myLaurel, a New York-based company that provides transitional and acute care to frail, elderly patients at home instead of a hospital. Patients received virtual and in-home visits from clinicians, along with lab work, medications, education about treatment plans and other services.”
- and
- “Cardinal Health has entered definitive agreements to acquire a majority stake in GI Alliance, a gastroenterology management services organization, and the entirety of Advanced Diabetes Supply Group, a diabetes medical equipment supplier.
- “Cardinal expects to acquire Advanced Diabetes Supply for an estimated $1.1 billion and 71% ownership of GI Alliance for an estimated $2.8 billion. Both deals are expected to close by early 2025, pending regulatory approvals.”
- STAT News relates
- “23andMe, the genetics startup that has repeatedly captured the public imagination and then faced nearly fatal business challenges, announced Monday that it would halt its efforts to develop new medicines and lay off 40% of its workforce, focusing instead on selling genetic tests to consumers and using the resulting data for research.
- “In closing its therapeutics division and laying off 200 people, 23andMe ended an audacious bet it made nearly a decade ago — that it could use the genetic data it had collected not only to assist drug companies but to become one itself.”
- Per Healthcare Dive,
- “General Catalyst released new details on its planned acquisition of Akron, Ohio-based Summa Health on Thursday, roughly one year after the venture capital firm said it was looking to buy a health system.
- “General Catalyst’s Health Assurance Transformation business, or HATCo, has signed a definitive agreement to purchase Summa for $485 million. The deal, alongside the health system’s current cash on hand, allows Summa to eliminate $850 million in debt — nearly all the debt the health system currently holds, according to Summa’s most recent financial results.
- “HATCo is also pledging to spend $350 million over the first five years of its ownership to support routine operations and technology investments, plus another $200 million over seven years for “strategic and transformative” initiatives.”
- Per MedTech Dive,
- “Johnson & Johnson said Tuesday it received an investigational device exemption (IDE) from the Food and Drug Administration to start a U.S. clinical trial for its Ottava surgical robot.
- “The company said it will now prepare U.S. sites to receive Ottava systems, enroll patients and begin surgical cases as it focuses on training clinical trial investigators. J&J’s soft tissue robot will compete with Intuitive Surgical’s da Vinci system, which currently leads the market.
- “The Ottava platform will incorporate J&J Ethicon surgical instruments designed for the robotic platform, the company said. Ottava will also have a digital system called Polyphonic that will connect surgical technologies, robotics and software, ultimately adding data and insights to support clinical decision making.”
- and
- “GE Healthcare has struck a deal to combine its Senographe Pristina mammography system with Radnet’s artificial intelligence-based Smartmammo workflow, the companies said Monday.
- “The alliance positions GE to distribute Radnet software designed to help mammography centers view images, prioritize cases and support other steps in the workflow. The integration is the first part of a broader collaboration focused on imaging AI.
- “Radnet CEO Howard Berger told analysts on an earnings call Monday that the mammogram systems “simply need a power source and a connection to the internet,” creating opportunities to image patients in “Walmart and mall locations.”