Midweek Update

In anticipation of tomorrow morning’s markup session, the House Appropriations Committee today released the draft Fiscal Year 2022 financial services and general government appropriations bill. Of note,
- Office of Personnel Management (OPM) – The bill includes $372 million, an increase of $42 million above the FY 2021 enacted level, for OPM to manage and provide guidance on Federal human resources and administer Federal retirement and health benefit programs.
- [The bill] eliminates provisions preventing the FEHBP from covering abortion services [subject to limited exceptions, e.g. life of the mother is endangered by continuing the pregnancy].
Govexec.com adds that “the bill makes no mention of a pay raise for federal employees, effectively endorsing [President] Biden’s plan to give feds an average 2.7% pay raise next year. It remains unclear how the White House would divvy up the 2.7% between an across-the-board increase to basic pay and an average increase in locality pay, although traditionally 0.5% has been reserved for locality pay increases.
From the COVID-19 front, the American Hospital Association informs us
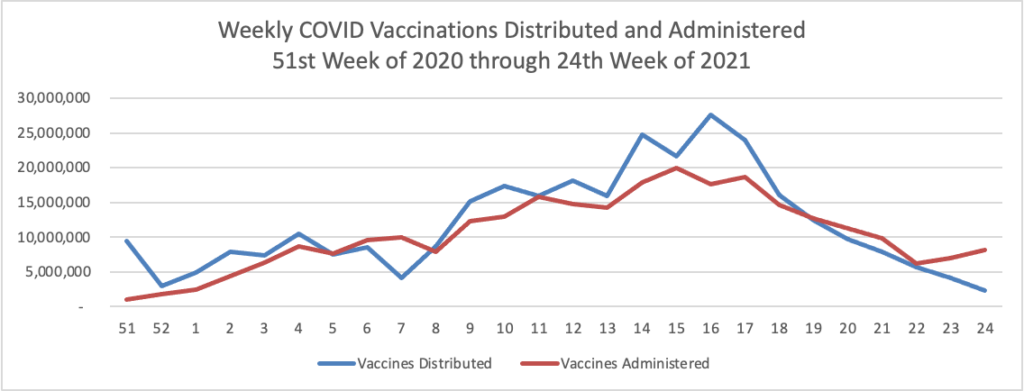
The AHA today joined the Department of Health and Human Services, Centers for Disease Control and Prevention, and other national health care and public health organizations in encouraging COVID-19 vaccination for everyone age 12 and older who is eligible. “Today, the CDC Advisory Committee on Immunization Practices (ACIP) met to discuss the latest data on reports of mild cases of inflammation of the heart muscle and surrounding tissue called myocarditis and pericarditis following COVID-19 vaccination among younger people,” the statement notes. “The facts are clear: this is an extremely rare side effect, and only an exceedingly small number of people will experience it after vaccination. Importantly, for the young people who do, most cases are mild, and individuals recover often on their own or with minimal treatment. In addition, we know that myocarditis and pericarditis are much more common if you get COVID-19, and the risks to the heart from COVID-19 infection can be more severe.”
Separately, the Food and Drug Administration today told ACIP that it was moving quickly to adjust the language on its emergency use authorization fact sheets for the Pfizer and Moderna COVID-19 vaccines to note a likely association in rare cases of myocarditis and pericarditis in vaccine recipients.
Bloomberg reports in this regard that
CDC Director Rochelle Walensky said Wednesday that mRNA vaccines have been successful in preventing severe illness and death among young people. For every million second doses of an mRNA vaccine administered to those 18-to-24-year-olds, the CDC projects 26,000 cases of Covid and 1,657 hospitalizations are prevented, while only 49 to 61 cases of myocarditis may develop. Speaking at the Milken Institute Future of Health Summit, Walensky added that the data presented at the advisory committee meeting still “overwhelmingly demonstrate that the benefits of vaccination far outweigh the risks.”
The Society for Human Resource Management offers advice on confronting COVID-19 vaccination misinformation in the workplace.
From the prescription drug front, Fierce Healthcare reports that employer groups are asking Congress to look into Biogen’s pricing of its new Alzheimer’s drug at $56,000 per course of treatment and the CVS Health continues to remove hyperinflationary drugs from its formularies in order to control drug spending.
Posaconazole, an antifungal medication, is priced at $4,500 for a 30-day supply—while an alternative, fluconazole, costs less than $14. This is an example of a growing trend: medications, including many generics, with “hyperinflated” prices, experts at CVS Caremark say. The pharmacy benefit manager giant culled 72 such drugs from its formulary in 2020 alone, leading to savings of $1.2 billion compared to 2018.
From the price transparency world, RevCycle Intelligence tells us that “The majority of the top 100 hospitals by gross revenue are using a price estimator tool to comply with a landmark hospital price transparency rule from HHS, according to a recent study.”
Finally, CIGNA has added a telemental service called Brightside to its behavioral health network. According to the provider’s press release,
Brightside, a mental health telemedicine platform that offers access to high-quality anxiety and depression care from anywhere, today announced that it has joined the national behavioral health network for Cigna Corporation, a global health service company. Cigna’s 14 million behavioral health customers can now access Brightside’s evidence-based and data-driven approach to treating anxiety and depression through their commercial health care plans.” * * * “The pandemic has shined a light on the need for broader, more convenient access to mental health care. Cigna is committed to providing our customers with the behavioral health care they need, when and where they need it – and that is what Brightside will help us offer,” said Dr. Doug Nemecek, Cigna’s chief medical officer for behavioral health. “By increasing access through virtual care, customers can talk to a psychiatrist or therapist from the comfort and privacy of their homes. This is another demonstration of our commitment to provide timely and convenient access to depression and anxiety care for Cigna members.
The FEHBlog appreciates such services because in contrast to in person care where the mental health providers are typically out of network, telemental providers in a spoke and hub arrangement like this one are always in-network, thereby creating savings for the plan and the member.