Tuesday Tidbits
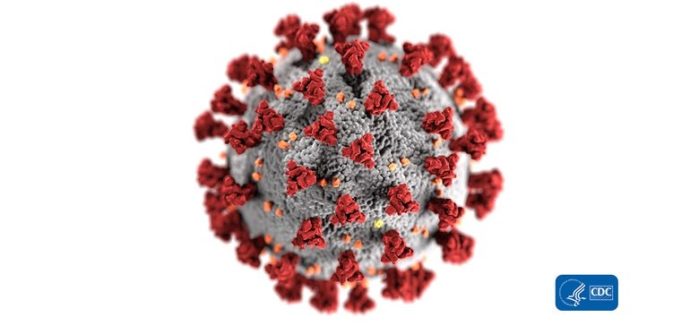
Good news! STAT News reports that “Moderna’s Covid-19 vaccine led patients to produce antibodies that can neutralize the novel coronavirus that causes the disease, though it caused minor side effects in many patients, according to the first published data from an early-stage trial of the experimental shot.” The FEHBlog will take it. What’s more, “The [Moderna] data roughly mirror the results from a similar vaccine being produced by Pfizer and BioNTech, which were released July 1.” Fingers remain crossed.
Healthcare Dive informs us about a FairHealth analysis which concludes that
The median charge for hospitalized COVID-19 patients aged 23-30 was about $35,000, while those aged 51-60 had median charges of about $46,000.
The most common other illness found in those patients is chronic kidney disease or kidney failure. Nationally, those patients accounted for 13% of all hospitalized COVID-19 patients during the study period from January to May. The second most common comorbidity in all but one region is Type 2 diabetes, according to the study that looked at private healthcare claims. The exception, the South, had hypertension in that rank.
The report also found the most common venue for an initial COVID-19 diagnosis nationally was a traditional doctor's office. About 33% of COVID-19 patients sought help from an office, while 23% went to an inpatient facility, such as an emergency room. In the Northeast, about 7% of COVID-19 diagnoses in that region came via telehealth appointments, versus 6.2% from ER visits.The Health Affairs Blog provides details on how the COVID-19 virus impacts people differently when viewed from a racial or ethnic perspective. These disparities deserve the attention of the healthcare industry.
We used data from the Medical Expenditure Panel Survey to explore potential explanations for racial-ethnic disparities in coronavirus disease 2019 (COVID-19) hospitalizations and mortality. Black adults in every age group were more likely than whites to have health risks associated with severe COVID-19 illness. However, whites were older on average than blacks. Thus, when all factors were considered, whites tended to be at higher overall risk compared to blacks, with Asians and Hispanics having much lower overall levels of risk compared to either whites or blacks. We explored additional explanations for COVID-19 disparities, namely differences in job characteristics and how they interact with household composition. Blacks at high risk of severe illness were 1.6 times as likely as whites to live in households containing health-sector workers. Among Hispanic adults at high risk of severe illness, 64.5 percent lived in households with at least one worker who was unable to work at home, versus 56.5 percent among blacks and only 46.6 percent among whites.
FYI, HealthIT.gov reports that at the request of Congress the federal government “is investigating strategies to improve patient identity and matching. Stakeholder input and insight into existing challenges and promising innovations in patient identity and matching will inform [Office of the National Coordinator of Health Information’s] ONC’s report to Congress on technical and operational methods that improve patient identity and matching. We invite all stakeholders to submit comments to identity.onc@hhs.gov by September 18, 2020.”
Supreme Court journalist Amy Howe reports that the U.S. Supreme Court has announced its oral argument calendar for October 2020. The calendar does not include the ACA constitutionality case, Texas v. California. The FEHBlog is willing to bet the ranch that the Supreme Court will uphold the ACA’s constitutionality (although it may remove the individual mandate from the statute which is what Congress intended when it zeroed out the individual mandate penalty).
In other litigation news, the FEHBlog discovered today that on August 3, 2020, at 2 pm, the U.S. District Court for the District of Columbia will hear oral argument on the Whitman-Walker Clinic’s motion to preliminarily enjoin enforcement of the recent HHS revised ACA Section 1557 rule. Section 1557 is the ACA’s individual non-discrimination provision. The FEHBlog is keeping an eye on this case.
Regrettably , Federal News Network reports that OPM has decided not to award any Presidential Rank award this year due to the disruptions created by the COVID0-19 emergency. The FEHBlog was honored ten years ago to participate in judging these awards. The FEHBlog was and remains very impressed by the work of the federal employees wh0 are nominated for these awards. Hopefully the awards which also were suspended for 2013 will return next year.