Friday Stats and More
Based on the Centers for Disease Control’s COVID Data Tracker and using Thursday as the first day of the week here is FEHBlog’s weekly chart of new COVID cases from the 27th week of 2021 through the second week of this year:

Four million new cases of COVID in a week. Wow. The Delta surge is the long hill that starts at the left of the chart. Omicron is Mount Everest by comparison.
Here’s the FEHBlog’s weekly chart of new COVID deaths for the same time span.

Weekly COVID deaths haven’t crossed 10,000 since the Delta surge peaked. Of course deaths are a lagging indicator.
The FEHBlog does think based on his reading that we are close to turning another corner but it’s not showing in these charts yet. We remain in the soup.
Here’s the FEHBlog’s chart of weekly Covid vaccinations distributed and administered since COVID shots were made available to the public in December 2020.

For the first time since before the holidays the number of administered vaccines, including boosters, exceeded 10 million last week. We are closing on 75% of the U.S. population aged 18 and older being fully vaccinated and over 65% of the U.S. population aged 65 and older being boostered.
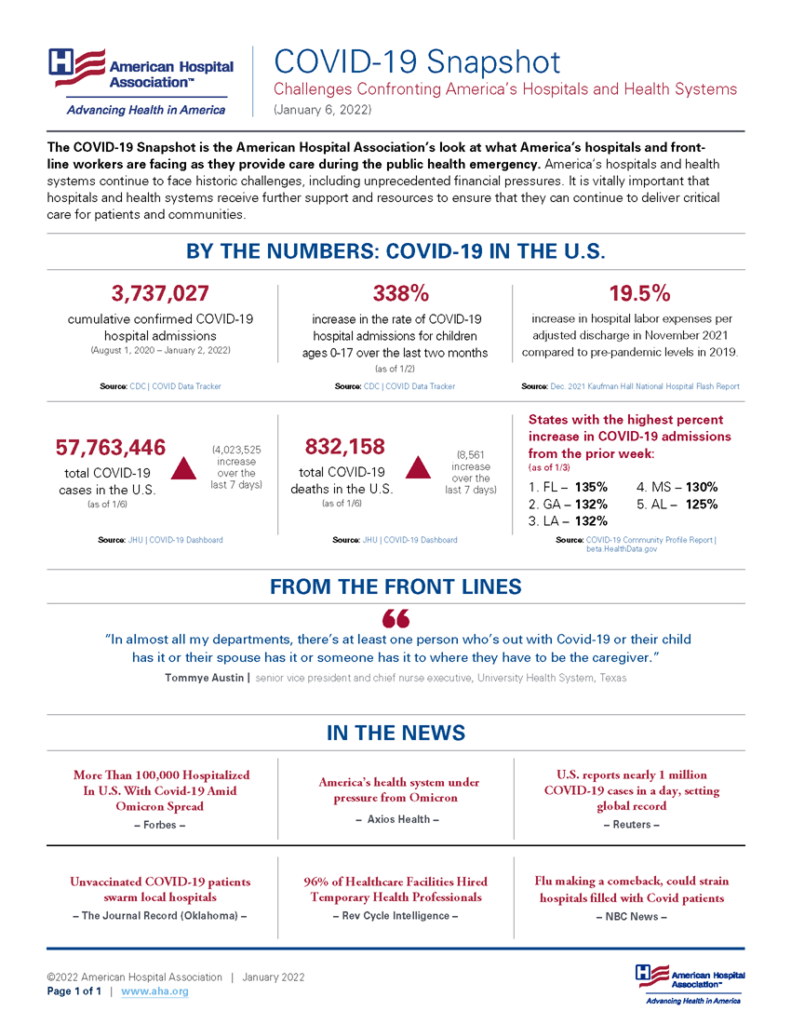
Here are links the the CDC’s interpretation of its recent Covid and Flu statistics. The American Hospital Association informs us that
As urged by the AHA, the Department of Health and Human Services today renewed the COVID-19 public health emergency declaration for another 90 days effective Jan. 16. The extension will help hospitals and health systems combat COVID-19 in their communities.
In the wake of the Supreme Court lifting the stay on the CMS healthcare worker stay mandate, the American Hospital Association explains
The Centers for Medicare & Medicaid Services today released updated interpretive guidance on its Omnibus COVID-19 Health Care Staff Vaccination Interim Final Rule for states affected by yesterday’s Supreme Court’s decision on the rule. The guidance does not apply to Texas, where the Interim Final Rule is still subject to a preliminary injunction in a separate legal action that was not before the Supreme Court. Under the guidance, the first dose compliance date for those states is Feb. 14, 2022, with full compliance expected from providers by March 15, 2022. For states not impacted by the Supreme Court decision, the previously announced compliance dates of Jan. 28 and Feb. 27 remain in effect. For both groups, the underlying interpretive guidance released on Dec. 28 applies and all members can still refer to the previously released Frequently Asked Questions for additional information.
Tomorrow is the implementation date for the President’s mandate that health plans cover over-the-counter COVID tests. It’s worth noting that health plans generally don’t cover any products sold over-the-counter so needless to say plans needed many more than the four days that federal govenment gave them to implement. The New York Times delves into the details.
The Wall Street Journal reports that
The U.S. public can begin ordering free at-home rapid Covid-19 tests through a new government website on Jan. 19, senior Biden administration officials said.
Initially, orders will be limited to four tests per residential address. Tests will ship via mail within 7-12 days of ordering, the officials said. The administration expects that timeline to shorten as the program ramps up, one of the officials said.
The public will be able to order tests at covidtests.gov. Those without access to the internet can place orders via phone, and the administration will work with community groups to help people request tests, the officials said. The government will give priority to orders from areas that have been hard-hit by the pandemic and low-income parts of the country.
Here’s a link to the White House’s fact sheet on these programs. Govexec discusses the Postal Service’s important role in distributing the tests ordered over the government website.
From the masking front, STAT News reports that
U.S. health officials on Friday encouraged more Americans to wear the kind of N95 or KN95 masks used by health-care workers to slow the spread of the coronavirus.
Those kinds of masks are considered better at filtering the air. But they were in short supply previously, and Centers for Disease Control and Prevention officials had said they should be prioritized for health care workers.Related: Comparing the Covid-19 vaccines developed by Pfizer, Moderna, and Johnson & Johnson
In updated guidance posted late Friday afternoon, CDC officials removed concerns related to supply shortages and more clearly said that properly fitted N95 and KN95 masks offer the most protection.
However, agency officials noted some masks are harder to tolerate than others, and urged people to choose good-fitting masks that they will wear consistently.
“Our main message continues to be that any mask is better than no mask,” Kristen Nordlund, a CDC spokeswoman, said in a statement.
In other news —
- Regulatory News informs us that “The Senate Health, Education, Labor and Pensions (HELP) Committee on Thursday voted 13-8 to advance the nomination of Robert Califf for a second stint as commissioner of the US Food and Drug Administration (FDA).”
- Precision Vaccines reports that
Researchers at Weill Cornell Medicine and the University of Oxford announced on January 10, 2022, their new study shows that common vaccines could help reduce the health burden of the COVID-19 pandemic.
A peer-reviewed study published in the Proceedings of the National Academy of Sciences crystallizes decades of evidence suggesting that the generalized immune-boosting properties of many vaccines can cross-protect people against multiple pathogens.
While these researchers did not specify particular vaccines, they chose values for cross-protection consistent with data from earlier studies on measles, influenza, tuberculosis, and other immunizations.
- Fierce Healthcare tells us that “A top Medicare advisory board [MEDPAC] did not recommend any new payment hikes for acute care hospitals or doctors for 2023, stating that targeted relief funding has helped blunt the impact of the COVID-19 pandemic.” We shall see.