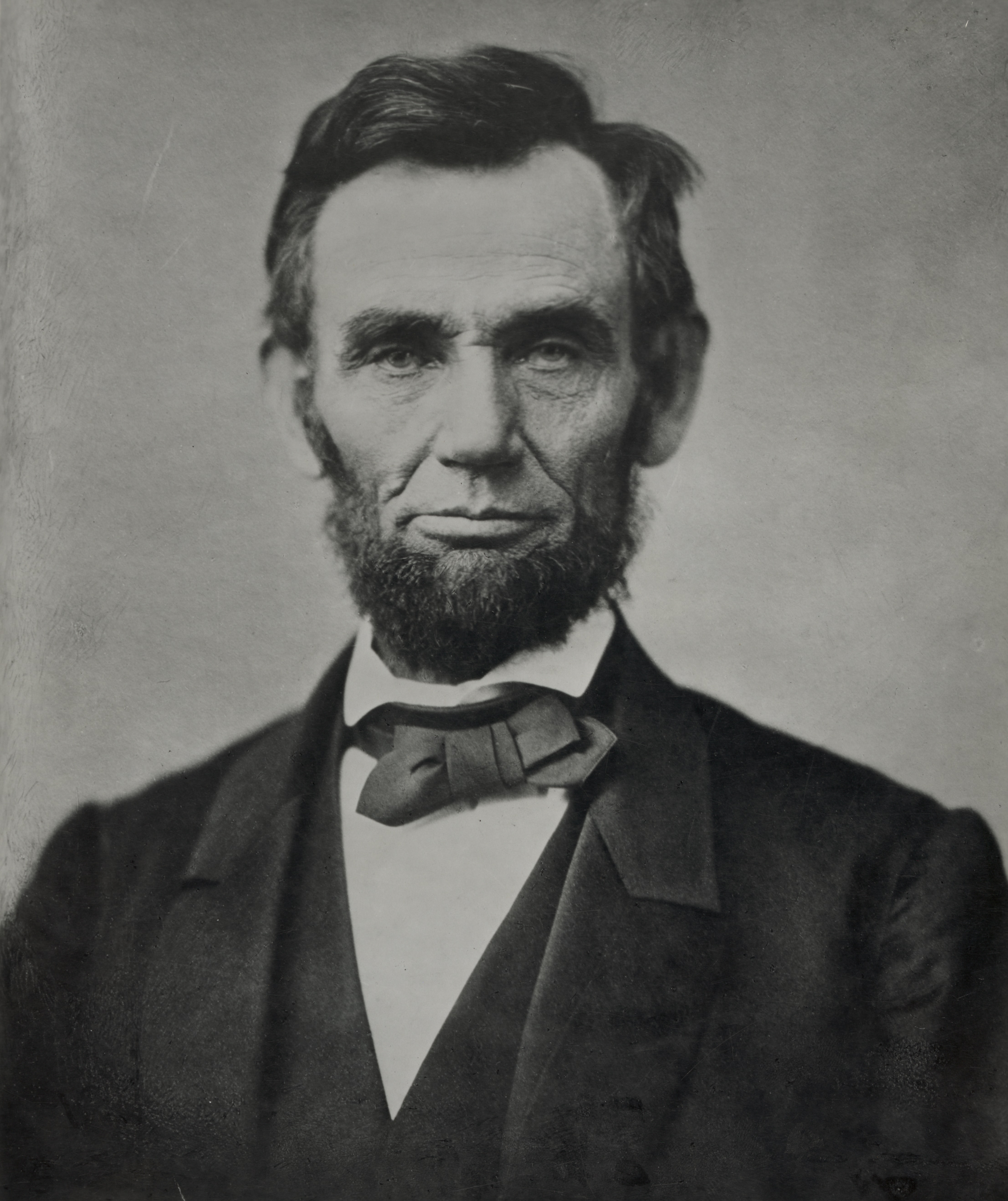
Happy Presidents’ Day

From Washington, DC
- The Senate and the House of Representatives are on recess until next week.
From the public health and medical research front,
- ABC News reports,
- “Half of all states are seeing high levels of respiratory virus activity, new federal data updated Friday shows.
- “Currently, 25 states plus New York City and Washington, D.C., are experiencing “high” or “very high” levels of respiratory illness activity, according to the Centers for Disease Control and Prevention (CDC).
- “While this is higher than the 23 states experiencing “high” or “very high” activity levels last week, it is fewer than the peak of 38 states reporting “high’ or ‘very high’ levels the week ending Dec. 30. * * *
- “Adults over age 65 continue to have the highest rates of both COVID and flu hospitalizations.”
- Fortune Well informs us,
- “Vaccines that protect against severe illness, death and lingering long Covid symptoms from a coronavirus infection were linked to small increases in neurological, blood, and heart-related conditions in the largest global vaccine safety study to date.
- “The rare events — identified early in the pandemic — included a higher risk of heart-related inflammation from mRNA shots made by Pfizer Inc., BioNTechSE, and Moderna Inc., and an increased risk of a type of blood clot in the brain after immunization with viral-vector vaccines such as the one developed by the University of Oxford and made by AstraZeneca Plc.
- “The viral-vector jabs were also tied to an increased risk of Guillain-Barre syndrome, a neurological disorder in which the immune system mistakenly attacks the peripheral nervous system.”
- and
- “They say anything men can do, women can do better—which may include reaping the health benefits of regular exercise. That’s according to a new study published today in the Journal of the American College of Cardiology.
- “An international team of researchers from the U.S. and China showed that women who exercise regularly have a significantly lower risk of an early death or a fatal cardiovascular event than men who do the same. On top of that, the advantage holds true even when women put in less effort.
- “The observational study, which analyzed the exercise habits of more than 400,000 U.S. adults, found that compared to being inactive, engaging in regular physical activity lowered women’s mortality risk by 24%. Men saw a 15% reduction in risk.
- “Women who worked out also had a 36% reduced risk of a fatal cardiovascular event, such as a stroke or heart attack, than their inactive peers. Among men, those who were physically active showed a 14% reduced risk.”
- The Washington Post reports,
- “About 1 in 4 U.S. adults 65 and older — more than 14 million people — suffer a fall each year, according to the Centers for Disease Control and Prevention.
- “Falls are the leading cause of injury among those 65 and older, even though not all falls result in an injury, the CDC says. About 37 percent of older people who have fallen have sustained an injury that required medical treatment or activity restrictions. For instance, the CDC reports that 95 percent of hip fractures result from a fall, and falls also are the most common cause of traumatic brain injuries.
- “The National Institute on Aging notes that the odds of falling increase with age, but falls often can be prevented. Standard suggestions include fall-proofing your home space (making sure all stairs have hand rails and are well-lit, eliminating most throw rugs and keeping walk spaces clutter-free), careful management of medications (especially those that can cause dizziness or confusion), having regular vision checks and staying as active as possible (including doing exercises to maintain strength and balance).”
- STAT News tells us,
- “Niacin, or vitamin B3, has long been a U.S. public health darling to the point that it is added, by law, to cereal products. But a new study published Monday in Nature Medicine points to a potentially concerning effect of an excess of the vitamin: It may increase the risk of cardiovascular disease.
- “The study looked into two cohorts of patients without active heart disease, 60% of whom were treated with statins, and found a strong association between a metabolic product of excess niacin and an increased risk of major adverse cardiovascular events such as a heart attack or stroke. One in four of the people in the study had excess niacin, which doubled their risk of major cardiovascular events to levels comparable with diabetes or a previous heart attack.
- “It’s a fairly sizable risk. It’s on par with what we consider other large risks,” said Stanley Hazen, the section head of preventive cardiology and cardiac rehabilitation at the Cleveland Clinic and senior author of the study. “This opens up the door; it lays the foundation for new studies and new interventions from both a diagnostic and therapeutic perspective to try to reduce inflammation and cardiovascular disease.”
- Per Medscape,
- “A plant-based diet, low in dairy and meat but rich in fruits, vegetables, grains, and nuts, can improve sexual and urinary health in patients treated for local prostate cancer, new research showed.
- “The findings, published on February 13, 2024, in the journal Cancer, bolster previous research showing plant-based diets can reduce the risk for recurrence and improve survivorship in men with prostate cancer.
- “The current study shows for the first time an association between eating more plant-based food with better scores for quality of life among patients diagnosed with prostate cancer,” Stacy Loeb, MD, a urologist in the Departments of Urology and Population Health at NYU Langone Health, in New York City, who led the research.”
- and
- Cefepime-taniborbactam was 22% more effective than meropenem, which is a current treatment for complicated urinary tract infections (UTIs) and acute pyelonephritis, according to a study published in The New England Journal of Medicine.
From the healthcare business front,
- The Wall Street Journal reports,
- “China has more obese people than anywhere else in the world, and they are increasingly turning to weight-loss drugs to solve the problem.
- “That is fueling a gray market of drug sellers and buyers, who have little trouble getting around China’s rules on the use of Ozempic.
- “Ozempic isn’t available for weight loss in the country, instead being reserved for the treatment of Type 2 diabetes. But users on e-commerce platforms are able to buy the shots, colloquially known as “miracle drugs,” simply by declaring they have been diagnosed with diabetes—without providing proof.
- “They aren’t getting a bad deal: On JD.com, a dosage of Ozempic retails for around $139. That is higher than its cost on the country’s national-insurance plan but much cheaper than the $970 some users pay in the U.S. each month. JD.com didn’t respond to requests for comment.”
- NPR Shots notes,
- “Bayer is the latest name-brand drugmaker to dip its toe into the world of Mark Cuban’s online pharmacy, Cost Plus Drugs.
- “The website offers drugs at steep discounts bypassing middlemen called pharmacy benefit managers. It mostly sells generics, but has been slowly adding brand name products as well.
- “Yaz birth control pills and Climara, a hormone patch for menopause, will both now be available for a fraction of their list prices, including Cost Plus’s standard 15% markup and shipping.
- “As I look at our partnership with Cost Plus, I really look at this as a test and learn,” says Sebastian Guth, president of U.S. Pharmaceuticals at Bayer. “It’s a first initial step. We will learn and see what the results of this partnership are and may then decide to expand it further.”
- Beckers Payer Issues points out,
- “Some health systems are getting out of the insurance business.
- “In the first weeks of 2024, two health systems announced plans to sell their health insurance subsidiaries. In February, Springfield, Mass.-based Baystate Health reached a deal to sell Health New England to Point32Health.
- “In January, Toledo, Ohio-based ProMedica said it planned to sell its insurance subsidiary, Paramount Health, to Medical Mutual of Ohio.
- “Baystate Health has around 180,000 members in Medicare, Medicaid and commercial, and Paramount Health has more than 77,000 members in Medicare Advantage, commercial, individual and short-term plans. Both are set to be acquired by larger nonprofit insurers. Point32Health and Medical Mutual of Ohio each have over 1 million members.”