Thursday Miscellany

From Capitol Hill, Roll Call reports
The Senate is expected to begin consideration of Democrats’ climate, tax and health care package on Saturday, leaving about two days for the party to shore up support for the bill.
Senate Majority Leader Charles E. Schumer said Thursday that he’s expecting a vote on the motion to proceed Saturday afternoon, which would follow a nomination vote he scheduled for 12:30 p.m.
The motion to proceed is a simple majority threshold; no Republicans are expected to back it.
If Democrats can secure the votes to move forward, it would trigger up to 20 hours of debate before a “vote-a-rama,” when senators can offer unlimited amendments and motions to delay the process. The debate time is equally divided between the parties and senators on either side can choose to yield back time in order to get to the vote-a-rama quicker.
It remained unclear Thursday afternoon whether party leaders had secured crucial backing from Sen. Kyrsten Sinema. * * *
Democrats are also working to wrap up the “Byrd bath,” in which the Senate parliamentarian hears arguments from both parties and issues opinions on whether provisions meet conditions of the budget reconciliation rules. Reconciliation allows the bill to avoid a filibuster and pass with only Democrats’ votes in the 50-50 Senate. * * * [Sen.] Sinema is expected to wait for the process to play out before making her position on the package known.
While the FEHBlog was writing this post, Politico reports
Sen. Kyrsten Sinema announced on Thursday night that she’s signed off on Democrats’ climate, tax and health care legislation after securing a handful of changes.
The Arizona Democrat was not consulted during July’s dealmaking between Senate Majority Leader Chuck Schumer and Sen. Joe Manchin, but after changes to several tax provisions she okayed the agreement on Thursday. “We have agreed to remove the carried interest tax provision, protect advanced manufacturing, and boost our clean energy economy in the Senate’s budget reconciliation legislation. Subject to the Parliamentarian’s review, I’ll move forward,” Sinema said.
From the Omicron and siblings front
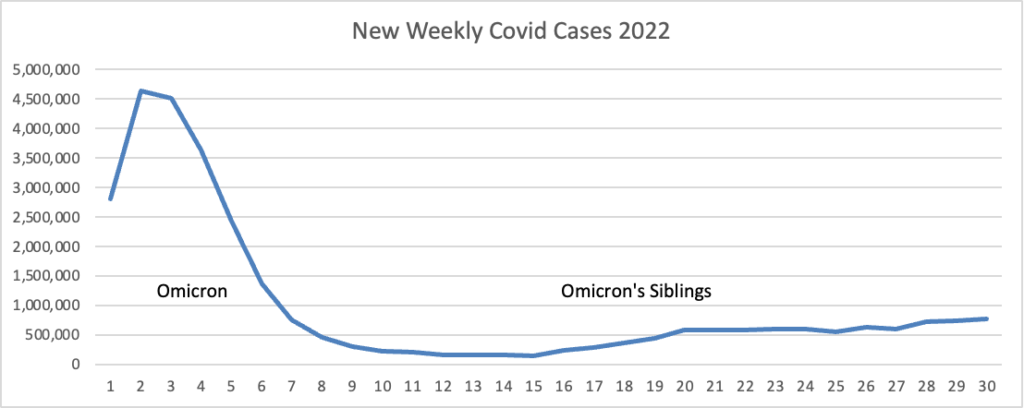
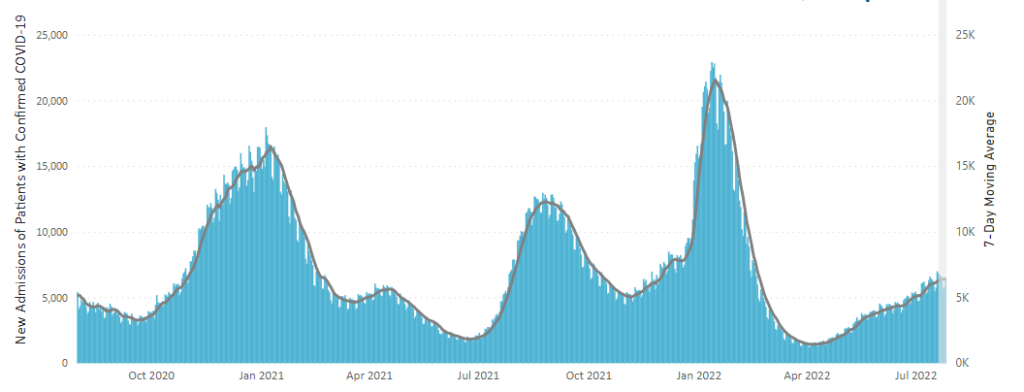
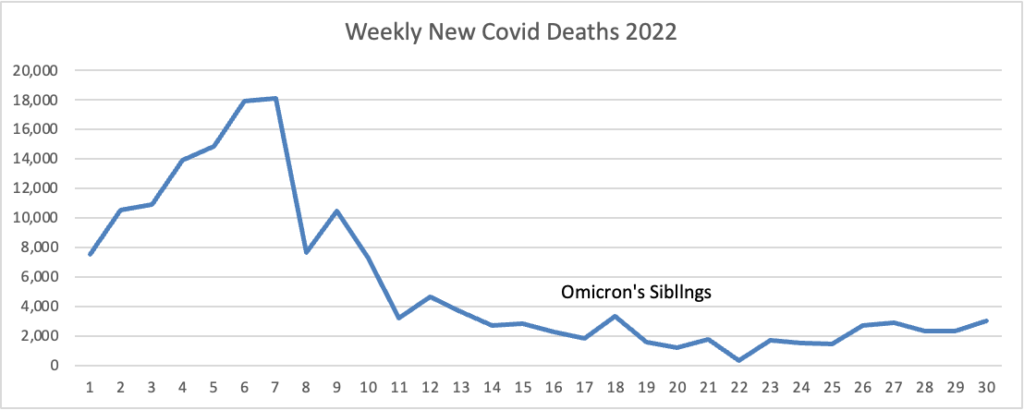
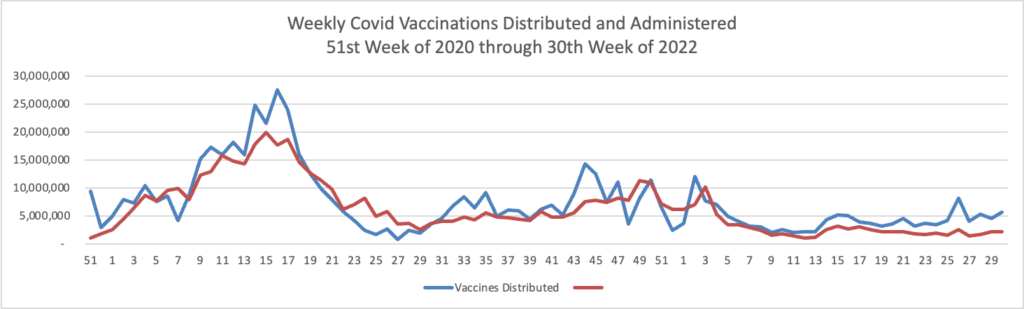
The New York Times explores the question “Is This What Endemicity Looks Like?” The article points out “The basic footprint of the disease has been consistent for a few months.”
We’ve been at roughly the same number of hospitalizations and deaths in the country since the end of the initial Omicron wave in the winter. And because so much of that has to do with how much better our immune systems are working against Covid than in the past, there’s probably no reason to think that those dynamics are going to dramatically change unless there’s an out-of-left-field new variant like the original Omicron.
And I think that fits the layperson’s understanding of what an endemic disease is: It’s circulating, but it’s sort of in the background, and while there are some little peaks and some little valleys, they aren’t so dramatic that they threaten to really upend life at a community level, let alone at a national level. That’s a pretty fair description of where we are right now.
While Omicron remains a dangerous virus, particularly for the elderly, which of course is where we started, we now have vaccines against severe illness and treatments for the virus.
It’s worth reading the article.
MedPage Today tells us
Most patients with smell or taste dysfunction related to COVID-19 reported complete recovery of their senses at 2 years, according to a cross-sectional survey conducted in Italy.
Among 119 patients with smell or taste dysfunction within 4 weeks of COVID onset, 88.2% reported complete resolution at 2 years, 9.2% reported a decline in symptom severity, and 2.5% reported unchanged or worsening symptoms, said Paolo Boscolo-Rizzo, MD, of the University of Trieste, and colleagues.
MedPage also offers us some Omicron miscellany
The CDC may relax guidance for COVID-19 control, including for schools, possibly as early as this week. (CNN)
And Los Angeles schools plan on updating COVID-19 protocols for the upcoming school year by dropping “overly aggressive” testing, masking, and vaccination requirements. (KTLA).
From the monkeypox front,
NPR reports
The White House today declared monkeypox a public health emergency.
“We are prepared to take our response to the next level in addressing this virus and we urge every American to take monkeypox seriously,” Health and Human Services Secretary Xavier Becerra said to reporters during a briefing on Thursday.
A public health emergency can trigger grant funding and open up more resources for various aspects of a federal response. It also allows the Secretary to enter into contracts for treatments and other necessary medical supplies and equipment, as well as support emergency hospital services, among other things. Public health emergencies last for 90 days but can be extended by the Secretary.
CDC Director Rochelle Walensky, said the declaration will provide resources and increase access to care. She also said it will expand the CDC’s ability to share data.
STAT News adds
Also Thursday, FDA Commissioner Robert Califf announced the agency was considering allowing Bavarian Nordic’s Jynneos, the only vaccine licensed in the United States to prevent monkeypox, to be given in two doses that are one-fifth the size of the licensed doses, via intradermal administration. Doing so could allow five times as many people to be vaccinated with existing supplies than if the licensed dosage was employed.
The vaccine is licensed as a two-dose product, with the doses administered via intramuscular injection 28 days apart.
“We believe this could be a promising approach,” Califf said.
In other public health news, the Department of Health and Human Services announced
Our nation’s blood and plasma supply dropped to historic lows during the COVID-19 pandemic. While some areas of the country have seen improvement, other areas are still struggling to meet the demand. Blood and plasma are needed on an ongoing basis to treat a variety of life-threatening conditions, which is why the U.S. Department of Health and Human Services (HHS), is launching a new campaign, Giving = Living. * * *
Visit hhs.gov/givingequalsliving to learn more about the importance of donation and make an appointment at a donation location near you.
From the U.S. healthcare business front —
Healthcare Dive tells us
Cigna reported net income increased 6% year over year to $1.6 billion during the second quarter as fewer people were admitted to the hospital, had fewer surgeries and visited the emergency room less.
The Connecticut-based insurer said medical costs for both COVID-19 and non-COVID-19 care were lower than projected. The insurer’s medical loss ratio, an important measure of how much is spent on medical care, fell to 80.7% for the second quarter. Analysts said price hikes helped the MLR, too.
As a result of the quarterly performance, Cigna raised financial targets for the year for revenue and income from operations.
Fierce Healthcare informs us
Telehealth company Amwell is working with CVS Health to roll out the retail drugstore giant’s new virtual primary care service.
CVS announced at the end of May plans to launch a virtual care service that gives consumers access to primary care, on-demand care, chronic condition management and mental health services. Eligible Aetna and CVS Caremark members will be able to use the virtual primary care service to access healthcare services on demand, whether at home or in a retail or community-based setting, the drug store company said.
CVS’ virtual care platform is a “consumer-centric offering designed to bring together the many elements of CVS Health ecosystem services into a single integrated experience with a unified digital front door,” Dr. Ido Schoenberg, chairman and co-chief executive officer of Amwell, said during the company’s second-quarter earnings call Thursday.
Elevance Health is betting big on primary care with a new nationwide partnership with Aledade.
The team-up will focus on assisting primary care practices in transitioning to value-based care, to boost health outcomes and lower costs. Independent primary care practices that are within the insurer’s network will be able to access Aledade’s suite of technology and local, in-person services.
Aledade’s platform provides the tools, support and resources that PCPs need to roll out value-based care, the companies said.
Bloomberg reports
Pfizer Inc. will spend $470 million to expand its vaccine research facilities 25 miles northwest of New York City, where the company hopes to maintain its edge in the booming field of messenger RNA, the technology behind its blockbuster Covid-19 shot.
The drugmaker will construct a new building and renovate existing facilities on its campus in Pearl River, New York, which has been the nexus of laboratory research driving its vaccine programs, including the one for Covid in partnership with BioNTech SE.
From the substance use disorder front, NPR explains
Music festivals once frowned upon naloxone, and some banned it. But even though what’s known as harm reduction — the concept of minimizing the negative effects of illicit drug use without trying to stop it altogether — has gained acceptance, it’s far from embraced. Less accepted than naloxone among concert promoters is helping people test their drugs for fentanyl. Companies don’t want to be seen as condoning drug use. They’re also navigating a legal gray area and battling public perceptions. * * *
Overdose deaths continue to climb in the U.S. Drug fatalities topped 100,000nationwide in 2021, with two-thirds caused by synthetic opioids. This has prompted federal and state governments to try to think of new ways to combat the crisis, with the Biden administration giving $30 million to support programs that have often operated in the shadows. In the past few years, the Substance Abuse and Mental Health Services Administration also has fully embraced fentanyl test kits.
Still, many communities far beyond music festival grounds are resistant to harm-reduction strategies, especially fentanyl-testing tools. Dr. Yngvild Olsen, director of SAMHSA’s Center for Substance Abuse Treatment, said harm reduction requires an evolution in thinking, and she encourages organizations to consider harm reduction a lifesaving tool — especially when mass overdoses are possible.
From the telehealth front, Health Payer Intelligence reports
Telehealth flexibilities during the coronavirus pandemic contributed to a 26 percent spike in overall utilization of in-network outpatient behavioral health, according to a report from UnitedHealth Group.
“Prior to the COVID pandemic, telehealth was broadly viewed as a potential strategy for improving access to behavioral health care,” the report explained.
“During the pandemic—which saw increased rates of depression, anxiety, and substance use disorder—federal and state policymakers and commercial health plans established temporary flexibilities to increase access to care, and patients and providers increased their use of virtual visits as an alternative to in-person office-based care.”