From Washington, DC,
- The Government Accountability Office informs us
- “Health care spending is higher in the U.S. than in any other high-income country. Yet, our health outcomes are worse.
- “It’s a tough issue to tackle. But when GAO faces tough policy challenges, the Comptroller General of the U.S. (and head of GAO) can convene a forum of experts to get their insights.
- Today’s WatchBlog post looks at our recent report about a forum on health care spending and quality of care.” * * *
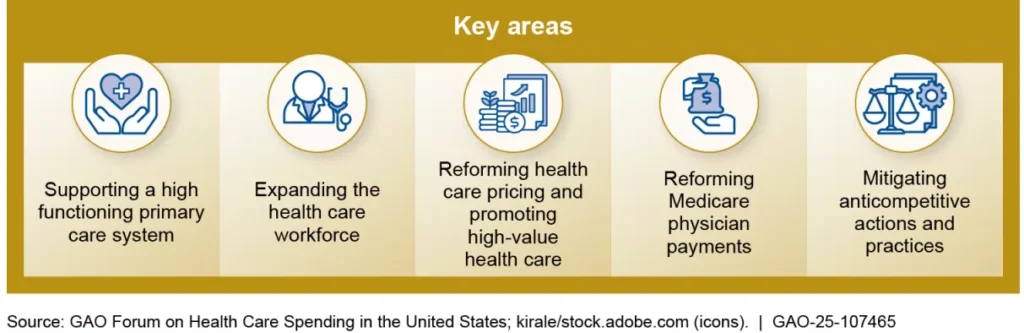
- During our forum on health care spending, experts from government, academia, and industry identified five key areas where—if action was taken—costs could be reduced and care improved. We provided approaches in these key areas to Congress in our report as potential options for addressing this issue.
- Politico reports,
- President Donald Trump plans to appoint Dan Scavino, a longtime loyalist and White House deputy chief of staff, to run the Presidential Personnel Office, empowering him with the power to decide who can and cannot serve in the administration.
- “Dan Scavino is one of President Trump’s most trusted and longest serving advisors,” said White House Press Secretary Karoline Leavitt. “There is nobody better to ensure the president’s administration is staffed with the most qualified, competent, and America First-driven workers. There is much still to be done and Dan’s leadership will ensure the highest quality, most dedicated workforce ever.”
- Health Affairs Forefront offers a No Surprises Act litigation status check written by Professor Katie Keith.
- “Nearly five years ago, President Trump signed the No Surprises Act into law, establishing new patient protections against surprise medical bills. Since the law took effect in 2022, millions of consumers have been protected from unexpected bills for out-of-network care—from emergency services to anesthesia to air ambulance rides. While the law has successfully protected consumers from the most common types of surprise out-of-network bills, its implementation has been hobbled by aggressive litigation.”
From the public health and medical research front,
- The Wall Street Journal reports,
- “Eli Lilly LLY said a third late-stage study of its experimental anti-obesity pill hit its key goals, paving the way for the drugmaker to begin regulatory submissions.
- “Eli Lilly on Tuesday said the Phase 3 study of orforglipron in adults with obesity or overweight and type 2 diabetes met the primary and all key secondary endpoints at all three doses, showing significant weight loss, meaningful A1C reductions and improvements in cardiometabolic risk factors at 72 weeks.
- “The Indianapolis company said study participants lost an average of 22.9 pounds, or 10.5% of their body weight, on the highest dose, with A1C, a measure of blood-sugar levels, reduced by an average of 1.8%.
- “Eli Lilly said orforglipron also showed a safety profile consistent with injectable GLP-1 medicines, such as its blockbuster Mounjaro and Zepbound drugs.
- “Eli Lilly said it now has the full clinical data package it needs to initiate global regulatory submissions for orforglipron this year.”
- BioPharma Dive adds,
- “An RNA medicine developed by Regeneron Pharmaceuticals and Alnylam Pharmaceuticals helped control symptoms of the chronic autoimmune disease generalized myasthenia gravis in adults enrolled in a late-stage study, Regeneron said Tuesday.
- “Regeneron also tested the RNA medicine, called cemdisiran, together with an antibody drug it developed and sells as Veopoz for another disease. However, study results suggested the combination was not as effective as cemdisiran alone.
- “Regeneron, which licensed cemdisiran from Alnylam, plans to submit the drug for U.S. approval in myasthenia gravis sometime in the first quarter next year. It is also testing the drug in paroxysmal nocturnal hemoglobinuria and geographic atrophy that is tied to age-related macular degeneration.”
- Genetic Engineering and Biotechnology News notes,
- “Germ cells pass DNA to the next generation and undergo massive reorganization of their DNA packaging to generate totipotency, or the ability to differentiate into any cell type. Understanding the mechanism of germ cell nucleome formation can offer valuable applications for addressing infertility.
- “In a new study published in Nature Structural & Molecular Biology titled, “The mitotic STAG3-cohesin complex shapes male germline nucleome,” researchers from Kyoto University have discovered STAG3-cohesin, a new mitotic cohesin complex that helps establish the unique DNA architecture of spermatogonial stem cells, which give rise to sperm. This discovery offers new strategies for treating infertility and certain cancers.”
- JAMA posted a research letter about “Trends in County-Level MMR [Measles, Mumps and Rubella] Vaccination Coverage in Children in the United States.”
- “Although the national- and state-level declines in MMR coverage are well documented, MMR vaccination coverage can vary substantially within a state.6 We generated a standardized dataset with annual county-level vaccination rates for children from 2017 to 2024 for all states in the US where this information was available and evaluated spatiotemporal trends in vaccination coverage during this period. This open, high-resolution dataset serves as a resource to explore the US vaccination landscape and its implications for vaccine-preventable disease.”
- Per MedPage Today,
- “Moderate-to-severe traumatic brain injury (TBI) increased malignant brain tumor risk in a large retrospective study of civilians.
- “This risk persisted when findings were meta-analyzed with data from two other cohorts.
- “The results echoed outcomes that emerged in an earlier study of young U.S. war veterans with TBI.”
- Consumer Reports, writing in the Washington Post, lets us know “what can make you dizzy? Could it be an inner-ear issue? Your medications? How to figure out the problem — and fix it.”
From the U.S. healthcare business front,
- Bloomberg Law reports,
- “Rising health-care costs are fueling the comeback of a strategy to limit hospital bills, but the evolving model requires employers to take on more work and risk in ditching the big insurance companies.
- “Reference-based pricing” typically determines a provider’s payments from Medicare rates, plus a premium ranging from 25-50%. Those rates fluctuate depending on the market and provider type, but advocates say they usually shave around 30% off a plan’s annual costs.
- “The strategy is part of employers’ ongoing search for alternatives to traditional health insurance as they confront an expected 9% spike in costs next year. But hospitals say RBP vendors are just middlemen looking to profit at patients’ expense.” * * *
- “The whole thing is very ugly from a patient perspective in the sense of it’s often not very clear what the rules are,” said Molly Smith, American Hospital Association’s group vice president for policy. “They often don’t understand whether or not they have a network.”
- “RBP companies blame the bad reputation on early iterations that sparked a series of lawsuits and left patients with steep bills. Many vendors today collaborate more with providers and protect patients, they said.
- “The differences in the models is how you deal with access issues, how do you deal with balance bills,” said Scott Ray, founder of RBP vendor 6 Degrees Health.”
- Modern Healthcare adds,
- “Concierge and direct primary care practices are gaining traction among physicians, employers and patients increasingly frustrated with traditional care pathways.
- “The growth of these practices, where patients pay membership fees in exchange for increased access to physicians, is a symptom of Medicare and Medicaid reimbursement that has not kept pace with inflation, advisers, doctors and policy experts said. Growing care backlogs, coding and documentation tasks that take doctors away from patients and seemingly ever-rising health insurance premiums are also contributing, they said.
- “A year ago, I would’ve told you these care models were a slowly evolving, quiet phenomenon,” said Dr. Zirui Song, an associate professor of healthcare policy at Harvard Medical School and a primary care provider at Massachusetts General Hospital. “It is now evolving quite rapidly — it is not so quiet anymore.”
- Beckers Hospital Review provides us with large for-profit healthcare system “payer mixes by patient service revenue, patient admissions or both in the first six months of 2025,” and tells us about three new drugs that OptumRx, a UnitedHealth subsidiary, is tracking this year.
- BioPharma Dive relates “Biopharmaceutical firms in the U.S. and Europe are increasingly turning to China’s biotech sector for new medicines. Follow this year’s dealmaking with this database.”
- Per Fierce Healthcare,
- “Health tech company Waltz Health will merge with Eversana with the goal of shaking up access to prescription drugs.
- “The deal will bring together Waltz’s proprietary drug marketplaces and direct-to-payer model with Eversana’s global pharmaceutical commercialization platform. In tandem, the two platforms will be well positioned to tackle the misaligned incentives in the drug supply chain and close gaps for patients, the companies said.
- “The combination will be especially critical in driving down the cost of pricey specialty pharmacy products, including GLP-1s, according to an announcement. Financial terms of the deal were not disclosed.”
- Per Modern Healthcare,
- “Independent laboratory company Quest Diagnostics and Corewell Health entered a definitive agreement to build a jointly owned lab in Michigan.
- “The Diagnostic Lab of Michigan would be based at the Corewell Health Southfield Center in Southfield, Michigan. It would focus on automated microbiology and high-throughput molecular testing.
- “Quest would also manage Corewell Health’s 21 inpatient and outpatient hospital labs as part of the joint venture. Financial terms were not disclosed.”
