Friday Stats and More
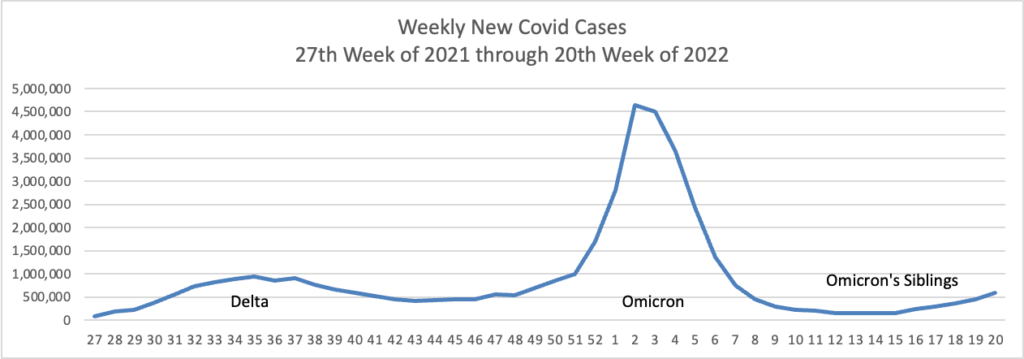
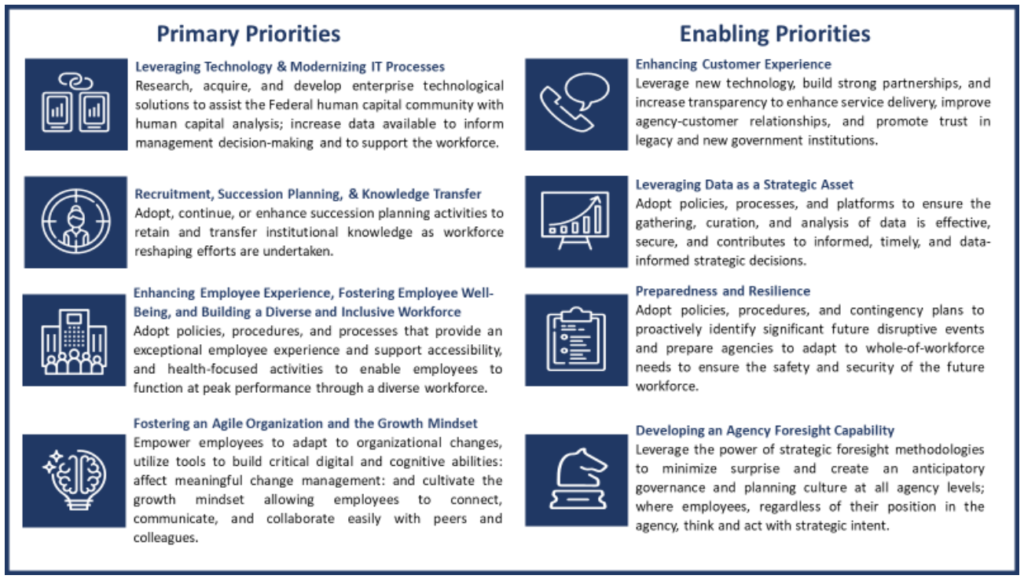
Based on the CDC’s Covid Data Tracker, and using Thursday as the first day of the week, here is the FEHBlog’s weekly chart of new Covid cases from the 27th week of 2021 through the 21st week of 2022:
The Wall Street Journal’s Numbers column observes
Reliable estimates of case counts are particularly relevant with the U.S. in the midst of yet another Covid-19 wave. By official case counts, it is a modest wave, at roughly 110,000 infections a day, according to the CDC. That is smaller than the 165,000 daily cases reported during the Delta wave, or the 250,000 a day during the 2020-21 winter.
But estimates of the true number of infections, correcting for undercounting, suggest the U.S. might be experiencing the second-largest wave of Covid-19 infections since the pandemic began.
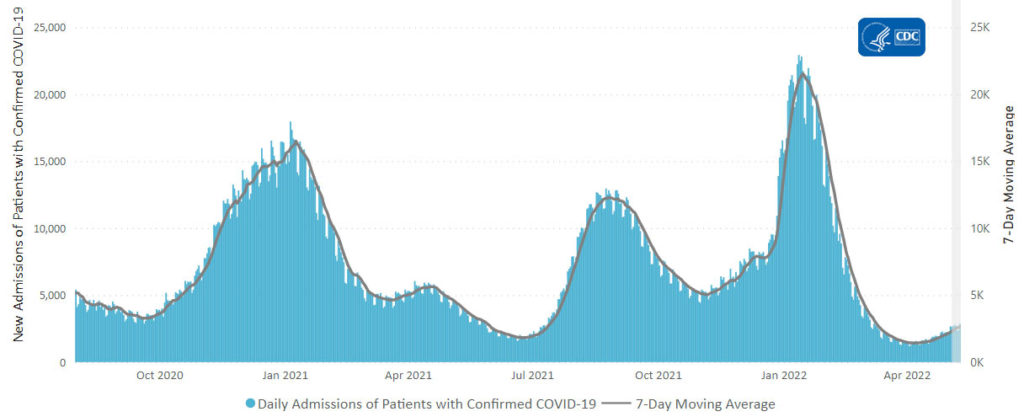
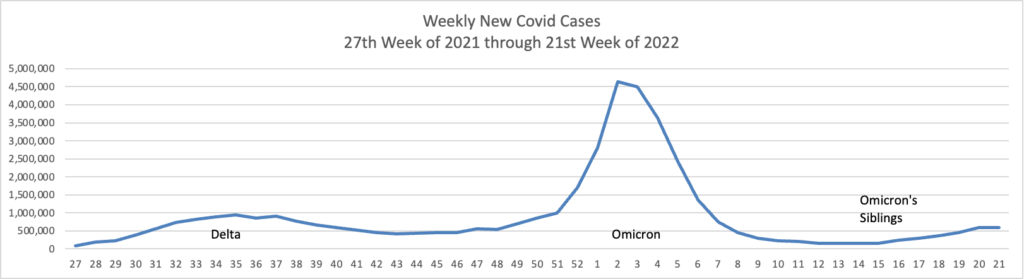
Here’s the CDC’s weekly chart of new Covid hospitalizations.
The Journal’s Numbers column notes
Hospitalization numbers also aren’t a perfect gauge. Someone can break a leg and test positive in the emergency room for a mild case of Covid-19. That case becomes a confirmed coronavirus hospitalization—and a strain on the hospital’s bed counts and personal-protective-equipment supplies—but not necessarily a severe case.
In Massachusetts, hospitals have begun reporting whether Covid-19 is the primary reason someone is in the hospital—and in January about 50% of cases were. It is hard to pinpoint how similar Massachusetts would be to other states, but it offers a further example of how better counting could improve assessment of the pandemic.
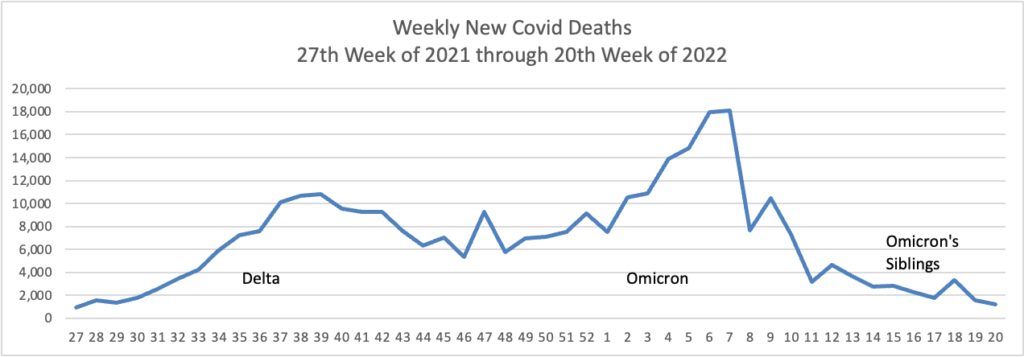
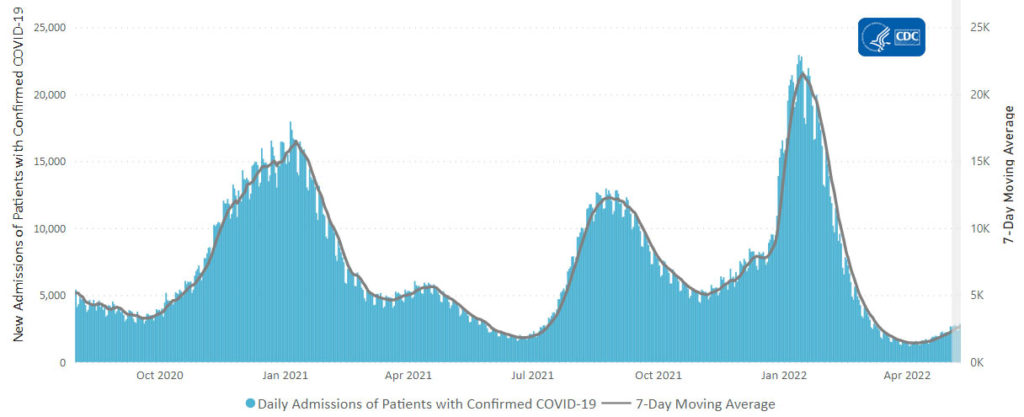
Here’s the FEHBlog weekly chart of new Covid deaths again from the 27th week of 2021 through the 21st week of 2022:
The Wall Street Journal reports
Covid-19 deaths in the U.S. are hovering near the lowest levels since the pandemic hit, showing how a population with built-up immune protection is less at risk of severe outcomes even as another wave of infections flows through the country.
The nearly 300 deaths reported daily are again more concentrated among older people, underscoring hazards for the more vulnerable while the overall population appears less at risk.
Particularly vulnerable people, such as those who are older and immunocompromised, will likely always have some risk of death from a Covid-19 infection, doctors and public-health experts said. Increasing booster rates and access to treatments, in addition to taking certain precautions, can help lower the threat presented by the virus, they said.
The New York Times adds
White House officials said on Thursday that they were introducing new models for distributing Paxlovid, the Covid-19 oral medication made by Pfizer, in an effort to get the treatment to more people and keep coronavirus death rates relatively low even as cases increase.
The federal government will start reimbursing a clinic in Providence, R.I., for evaluating patients who test positive and immediately prescribing Paxlovid to those eligible for it — the first of what the White House said would be a series of federally supported sites, with others set to open in New York and Illinois. Federal workers are also being sent to state-run testing sites in Minnesota, transforming them into “test-to-treat” locations, the White House said.
“Fundamentally, what we’re trying to do is get to a point where Covid deaths are largely preventable, and I think we’re pretty close to there,” Dr. Ashish K. Jha, the White House Covid-19 response coordinator, said in an interview Wednesday evening. “Deaths from this disease really should become increasingly rare.”
STAT News offers an interesting look into how scientists assess the level of Covid resistance to Paxlovid.
Resistance is the hobgoblin of antiviral medicine, even with antivirals as effective as Paxlovid. After doctors deployed nearly every new virus-killing infusion or pill in history, strains popped up — either immediately or eventually — with machinery warped in just the right way to evade the threat.
Exactly how much of a problem resistance will be for Paxlovid is complicated. In some patients, the coronavirus will inevitably find ways to evade the pill, as it did prior Covid-19 drugs.
“If there is anything we know about viruses and antiviral drugs is that eventually we will see some sort of resistance,” Andrew Pavia, chief of pediatric infectious diseases at University of Utah Health, said in an email.
What’s less clear, Pavia and other experts say, is whether any resistant variants will spread widely. The coronavirus may have particular difficulty getting around Paxlovid compared to other drugs because patients take it for only five days and because it targets a protein the virus can’t easily change. Any mutation or modification the virus makes may impair its ability to replicate or survive.
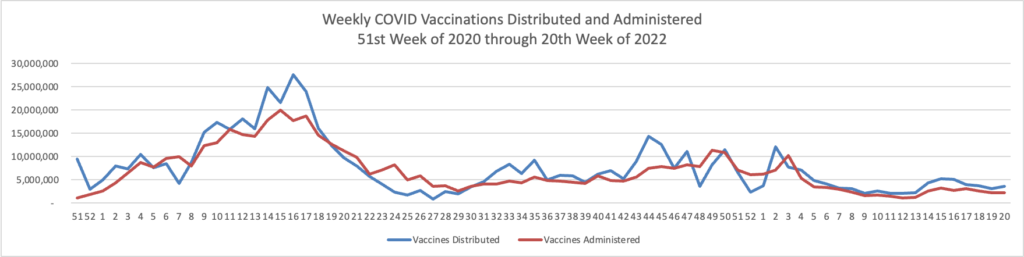
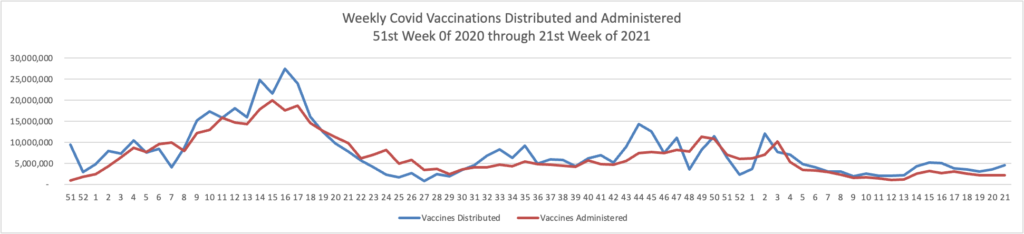
Here’s the FEHBlog weekly chart of Covid vaccinations distributed and administered
The CDC’s weekly review of its Covid statistic tells us
People who are up to date on vaccines have much lower risk of serious illness and death from COVID-19 compared with people who are unvaccinated. CDC’s COVID Data Tracker shows that in March 2022, adults ages 18 years and older who were unvaccinated were about 5 times more likely to be hospitalized with COVID-19 than those who were up to date. In the same month, people ages 12 years and older and unvaccinated were 17 timesmore likely to die of COVID-19 than those who were up to date.
COVID-19 vaccines available in the United States are effective at protecting people from getting seriously ill, being hospitalized, and even dying—especially people who are boosted. As with other diseases, you are protected best from COVID-19 when you stay up to date with recommended vaccines. Find a vaccine provider near you.
The CDC’s weekly review further explains
As of May 19, 2022, there are 301 (9.35%) counties, districts, or territories with a high COVID-19 Community Level, 477 (14.81%) counties with a medium Community Level, and 2,442 (75.84%) counties with a low Community Level. This represents a moderate (+5.10 percentage points) increase in the number of high-level counties, a slight (−0.74 percentage points) decrease in the number of medium-level counties, and a corresponding (−5.84 percentage points) decrease in the number of low-level counties. Five (9.62%) of 52 jurisdictions had no high- or medium-level counties this week.
To check your COVID-19 Community Level, visit COVID Data Tracker.
In big Medicare news
the Centers for Medicare & Medicaid Services (CMS) released a report that recommends cost savings from lower-than-expected Medicare Part B spending be passed along to people with Medicare Part B coverage in the calculation of the 2023 Part B premium. Earlier this year, Department of Health and Human Services (HHS) Secretary Xavier Becerra instructed CMS to reassess the 2022 Part B premium amount in response to a price reduction for Aduhelm™, a monoclonal antibody directed against amyloid for use in treating Alzheimer’s disease. Given the information available today, it is expected that the 2023 premium will be lower than 2022. The final determination will be made later this fall.
This CMS decision is quite sensible, in the FEHBlog’s view.
On a related FEHB note, FedSmith discusses the pros and cons of enrolling in Medicare Part B when you are a federal or Postal annuitant with FEHB coverage in retirement as well.
From the telehealth front, mHealth Intelligence reports
CVS Health has launched a new virtual care solution to create a more coordinated healthcare experience for consumers.
Called CVS Health Virtual Primary Care, the digital care platform will provide healthcare consumers with an array of care services, including primary care, on-demand care, chronic condition management, and mental health services. Consumers will also be able to choose their healthcare setting from various retail, community-based, virtual, and at-home care options.
“We’re meeting people where they are on their healthcare journey and providing care that is more convenient and easier to access,” said Creagh Milford, DO, vice president, enterprise virtual care at CVS Health, in the news release.
The new benefit will launch on January 1, 2023.
From the Rx coverage front, Formulary Watch reveals that
The Institute for Clinical and Economic Review (ICER) has released the protocol for its second annual review of insurance company policies to assess fair access to prescription drugs. ICER will evaluate whether 15 large U.S. commercial payers, the two largest state health exchange plans, and the Department of Veterans Affairs have formularies and procedures that provide appropriate access to the prescription drugs reviewed by ICER in 2020. These drugs include those that treat patients with cystic fibrosis, hemophilia A, migraine, sickle cell disease, and ulcerative colitis.
The analysis is expected to be completed in November 2022.
From the studies front, the Centers for Disease Control issued its 2021 Diabetes Report Card this week. Here are the highlights
* After almost 2 decades of continual increases, the incidence of newly diagnosed cases of diabetes in the United States decreased from 9.3 per 1,000 adults in 2009 to 5.9 per 1,000 adults in 2019.
* Prevalence of prediabetes among US adults remained steady from 2005–2008 to 2017–2020. However, notification of prediabetes status nearly tripled (from 6.5% to 17.4%).
* American Indian or Alaska Native, non-Hispanic Black, Hispanic, and non-Hispanic Asian people are more likely to be diagnosed with diabetes than non-Hispanic White people (14.5%, 12.1%, 11.8%, 9.5%, and 7.4%, respectively).
* During the COVID-19 pandemic, diabetes emerged as an underlying condition that increases the chance of severe illness. Nearly 4 in 10 adults who died from COVID-19 in the United States also had diabetes.