Tuesday’s Tidbits

The FEHBlog nearly fell off his office chair when he noticed a Govexec headline this afternoon reading “The House finally plans to vote on Postal reform [HR 3706] next week. The long sought after bill could make it to the President’s desk by the end of the month.” This Postal reform saga has been going on for over a decade.
The Postal reform act (HR 3706) would relieve the Postal Service of the obligation to prefund the cost of FEHB coverage in retirement for its employees. The bill also would create a Postal Service Health Benefits Program (“PSHBP”) within the FEHB Program. The PSHBP would tightly integrate Medicare annuitant coverage with primary Medicare A, B, and D. Medicare Part A (hospital care) is premium free while Medicare Part B (medical care) and Part D (prescription drugs) charge premiums.
OPM encourages Medicare age annuitants to pick up Part B but it prohibits FEHB carriers from using integrated Part D arrangements knowsn as EGWPs even though every other U.S. employer that provides drug coverage to its retirees uses a Part D EGWP or takes the retiree drug subsidy. What’s more Congress in the Medicare Modernization Act of 2003 expressly authorized FEHB plans to use Medicare EGWPs. Go figure.
In any event, all enrollee costs are included in FEHB risk pools which is an important feature of the FEHB Plan and its constituent PSHBP. The cost of Medicare Prime annuitants in the PSHBP will be much lower than those in legacy FEHB, and Medicare Prime annuitants are a signficant cadre of enrollment, PSHBP premiums will be noticeably lower than legacy FEHB premiums.
The CBO has projected that 3/5s of the Medicare integration savings for the PSHBP will come from the Part D EGWPs. The FEHBlog looks forward to the day later this decade when OPM finally permits legacy FEHB carriers to offer Medicare Part D EGWPs.
From the Covid vaccine front —
- Pfizer and BioNTech have a submitted an emergency use authorization request for an mRNA Covid vaccine for little children aged six months through four years. The FDA and CDC are likely to approve the application by the end of February according to Medscape.
- Medscape also informs us that
Novavax announced Monday that it has formally submitted a request to the FDA for emergency use authorization of its COVID-19 vaccine for ages 18 and older.
The request includes results from two large clinical trials that showed an overall efficacy of about 90% and a “reassuring safety profile,” the company said.
“We believe our vaccine offers a differentiated option built on a well-understood protein-based vaccine platform that can be an alternative to the portfolio of available vaccines to help fight the COVID-19 pandemic,” Stanley Erck, the president and CEO of Novavax, said in the statement.
From the COVID treatment front, the Wall Street Journal reports that providers are having difficulty obtaining the drugs need to treat Omicron because the treatments typically are available under emergency use authorizations and each State makes its own decison on how to distribute EUA treatments. On the brighter side,
Antiviral-pill manufacturers are ramping up production to meet demand. Supplies of Pfizer Inc.’s Paxlovid are expected to increase in the spring, according to Pfizer and state officials. Merck & Co., which manufactures molnupiravir with partner Ridgeback Biotherapeutics LP, said it has delivered two million courses to the U.S. and will deliver the rest of the 3.1 million courses under its contract by the end of this week.
From the healthcare cost front, Healthcare Dive reports that
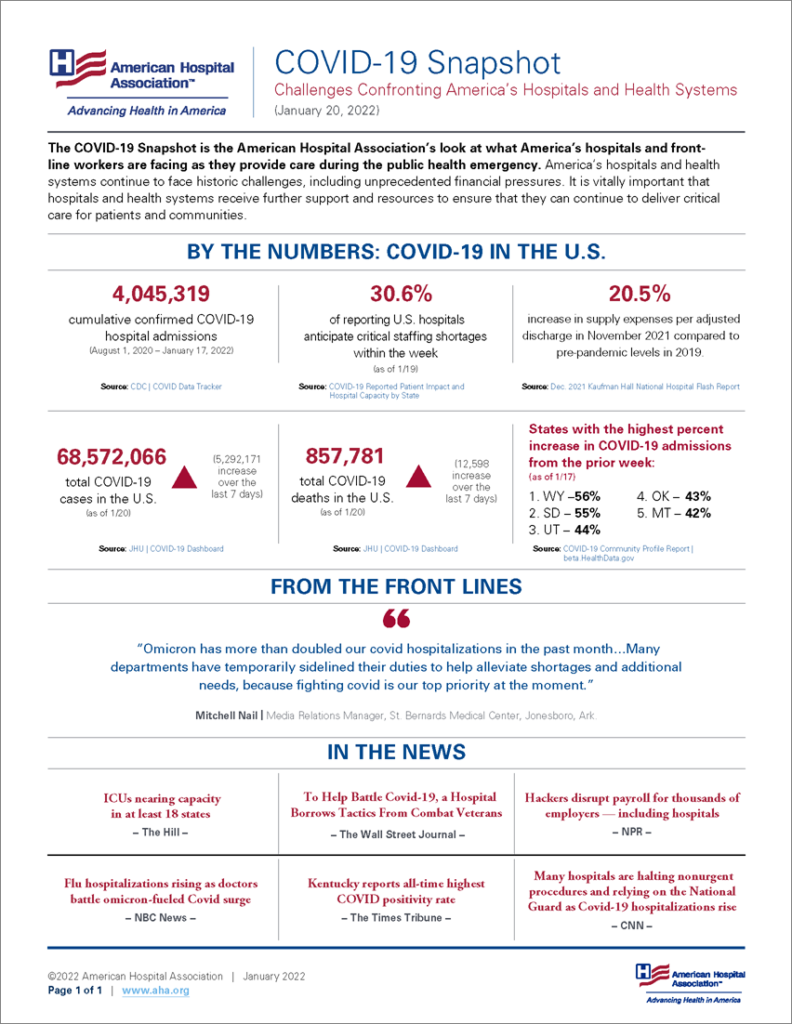
The omicron variant walloped hospitals in the final month of 2021, driving up both adjusted patient volumes and expenses as the number of COVID-19 cases surged to new highs for the pandemic, according to Kaufman Hall’s latest flash report.
Patient days rose nearly 4% in December compared to November, while emergency department visits jumped more than 7% as patients came in with COVID-19 symptoms. Omicron’s rapid spread drove a 98% jump in COVID-19 hospitalizations over the course of the month, Kaufman Hall said, citing Centers for Disease Control and Prevention data.
The second full year of the pandemic was marked by an increase in severely ill patients requiring longer hospital stays compared to the first year, the report also found.
From the No Surprises Act front, Healthcare Dive examines healthcare provider association legal challenges to the federal regulators’ use as the qualifying payment amount in NSA arbitrations. The FEHBlog has described those cases now pending in federal district courts in Texas and Washington DC as exercises in futility. For example,
Since the qualifying payment amount represents the median in-network rate, it by definition means that half of providers are below the QPA and half are above, according to Chris Garmon, a professor at University of Missouri – Kansas City, who has studied surprise billing. Not all providers are set to see payments decline and some may even see them increase if the QPA is used, he said.
The good professor overlooks the fact that in 2021 out of network doctors caring for patient at in-network facilities were reimbursed at out-of-network rates typically two or perhaps three times the Medicare RBRVS reimbursement. For that reason, the FEHBlog expects that in most cases the QPA will be noticeably higher than pre-NSA reimbursements. Time will tell, but the regulators’ approach is reasonable, and patient advocacy groups have been supporting the regulators in these cases.
From the mental health parity front, Health Payer Intelligence compares provider and payer reactions to the government’s recent report to Congress on payer compliance with complex federal health parity act rules.
From the healthcare business front, Fierce Healthcare tells us that
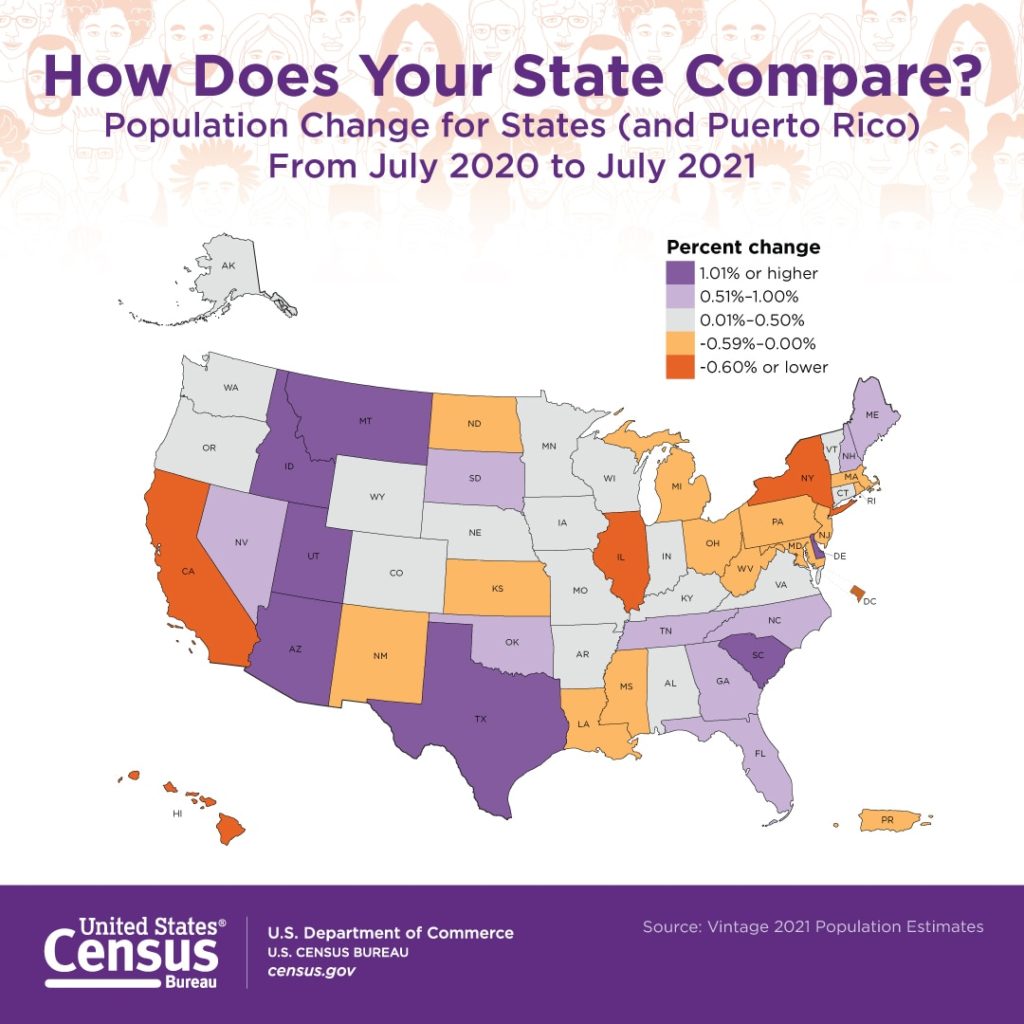
GuideWell, the parent company of Blue Cross and Blue Shield of Florida, has closed its acquisition of Triple-S Management Corporation, a Puerto Rico-based health services company.
The deal was first announced in September.
GuideWell acquired all shares of Triple-S at $36 per share in cash, according to an announcement from the company. Triple-S will now operate under its existing branding as a wholly owned subsidiary of GuideWell.
From the FDA front, check out this FDA news roundup.
From Capitol Hill, Govexec reports on OMB acting director’s Shalonda Young’s confirmation hearings to be the Presidentially nominated OMB director. Ms. Young appears on her way to confirmation.