Friday Stats and More
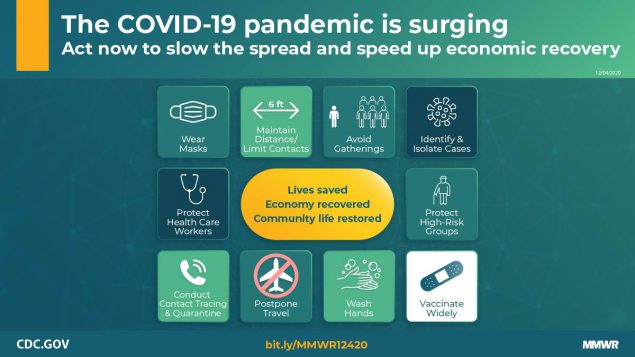
Based on the Centers for Disease Control’s COVID-19 Data Tracker website, here is the FEHBlog’s chart of new weekly COVID-19 cases and deaths over the 14th week of 2020 through 9th week of this year (beginning April 2, 2020, and ending April 7, 2021; using Thursday as the first day of the week in order to facilitate this weekly update):
and here is the CDC’s latest overall weekly hospitalization rate chart for COVID-19:

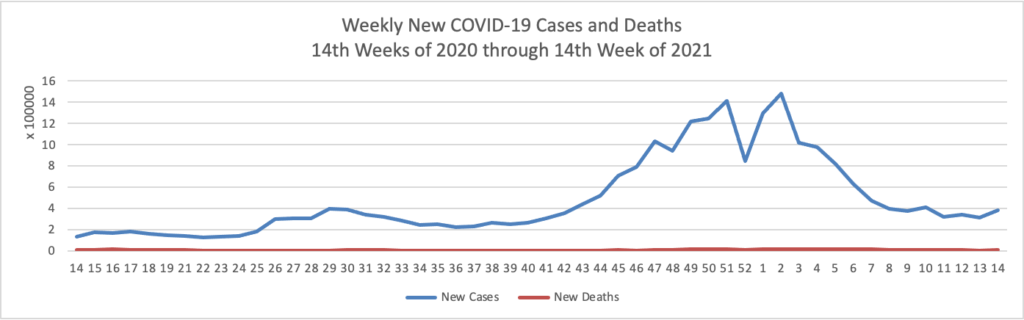
The FEHBlog has noticed that the new cases and deaths chart shows a flat line for new weekly deaths because new cases greatly exceed new deaths. Accordingly here is a chart of new COVID-19 deaths over the period (April 2, 2020, through April 7, 2021):
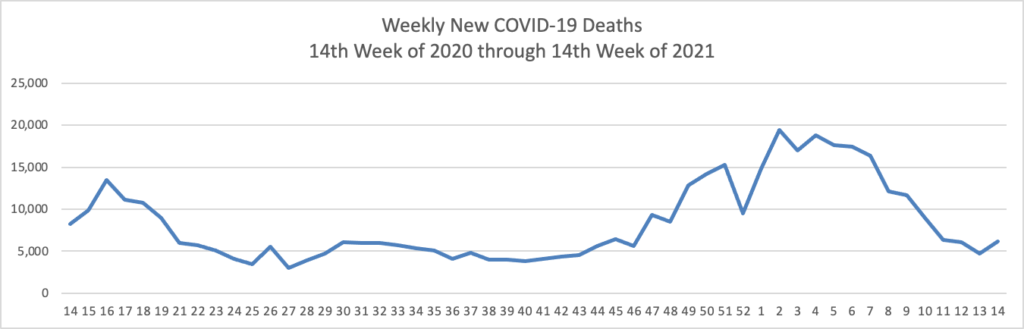
Finally here is a COVID-19 vaccinations chart over the period December 17, 2020, through April 7, 2021 which also uses Thursday as the first day of the week:
That is quite a sharp increase in distributed doses of the COVID-19 vaccine.
Bloomberg reports that
The U.S. recorded 4 million vaccine doses on Friday, returning the pace of inoculations almost to the level before a post holiday lull, according to the Bloomberg Vaccine Tracker. It was the third straight day of increases, with the seven-day average now at 3.03 million doses a day. So far, 179 million doses have been administered. At this pace, it’s estimated to take another 3 months to cover 75% of the population.
Pfizer and BioNTech announced today that they have “requested amendments to the U.S. Emergency Use Authorization (EUA) of the Pfizer-BioNTech [2 dose mRNA] Vaccine (BNT162b2) to expand the use in adolescents 12 to 15 years of age.” That’s a good sign for an in-person teaching in high schools next year.
Bloomberg also reports this evening that
The U.S. Centers for Disease Control is working with health departments in four states to evaluate symptoms experienced after Johnson & Johnson vaccinations but has “not found any reason for concern,” a spokeswoman said in a statement.
“Many people don’t have any side effects after Covid-19 vaccines, but some people will have pain or swelling at the injection site or fever, chills, or a headache,” spokeswoman Kristen Nordlund said. “These typically don’t last long and are signs that your body is building protection.”
She said the states are Colorado, North Carolina, Georgia and Iowa. The symptoms include “dizziness, light headedness, feeling faint, rapid breathing, and sweating.” She said the CDC “is aware of other instances of these symptoms occurring with the other Covid-19 vaccines.”
The Wall Street Journal cautions that “Deliveries of Johnson & Johnson’s JNJ -1.06% Covid-19 vaccine doses throughout the U.S. are expected to plunge by more than 80% next week, according to state officials and federal data, as J&J grapples with manufacturing challenges.”
Whither the emergency use application for the other adenovirus based COVID-19 from AstraZeneca/Oxford University?
Under the and More subheading —
- Yesterday the CDC Director Rochelle Walensky issued a statement on her “Commitment to Addressing Racism as an Obstacle to Health Equity.” “To build a healthier America for all, we must confront the systems and policies that have resulted in the generational injustice that has given rise to racial and ethnic health inequities. We at CDC want to lead in this effort—both in the work we do on behalf of the nation’s health and the work we do internally as an organization.” Well said.
- The Biden Administration released an abbreviated version of its Fiscal Year 2022 federal budget today.
The Office of Management and Budget (OMB) today submitted to Congress President Biden’s discretionary funding request for Fiscal Year 2022. As Congress prepares to begin the annual appropriations process, the request lays out the President’s discretionary funding recommendations across a wide range of policy areas and outlines a strategy for reinvesting in the foundations of our country’s resilience and strength. The request — which represents only one element of the Administration’s broader agenda — includes key investments in K-12 education, medical research, housing, civil rights, and other priorities that are vital to our future. Later this spring, the Administration will release the President’s Budget, which will present a unified, comprehensive plan to address the overlapping challenges we face in a fiscally and economically responsible way.
The Wall Street Journal adds that “The preliminary plan released Friday by the White House would raise discretionary spending by 8.4%, or $118 billion, from the $1.4 trillion authorized last year, excluding emergency measures to combat the Covid-19 pandemic. Discretionary spending is the part of the budget that Congress shapes through the appropriations process.”
- Yesterday, the FEHBlog discussed the Center for Medicare and Medicaid Service’s proposal rule for the Fiscal Year 2022 Medicare prospective payment and quality system for psychiatric hospitals. Becker’s Hospital CFO Report informs us that in addition CMS issued three other pricing rules for rehabilitation hospitals, hospices, and skilled nursing facilities.
- Finally, Fierce Healthcare reports that
While hospitals post a mixed record on complying with a major price transparency rule [that took effect on January 1, 2021],the Biden administration has not announced how they are going to keep facilities in line.
Several studies and analyses have shown that larger health systems have not done a good job fully complying with the rule to post payer-negotiated rates online. The results come as the Centers for Medicare & Medicaid Services (CMS) has not announced major enforcement actions against hospitals not meeting the controversial rule’s requirements.
“So far with the current administration, we haven’t seen the agency put out any information on the auditing process or changes to the reporting requirements or changes to the penalties for noncompliance,” said Caitlin Sheetz, director and head of analytics for consulting firm ADVI, in an interview with Fierce Healthcare. “Unless that changes, I don’t think we are going to see large shifts in hospital behavior.”