Weekend update

Happy Law Day 2022!
The House of Representatives and the Senate will be engaged in Committee business and floor voting this week.
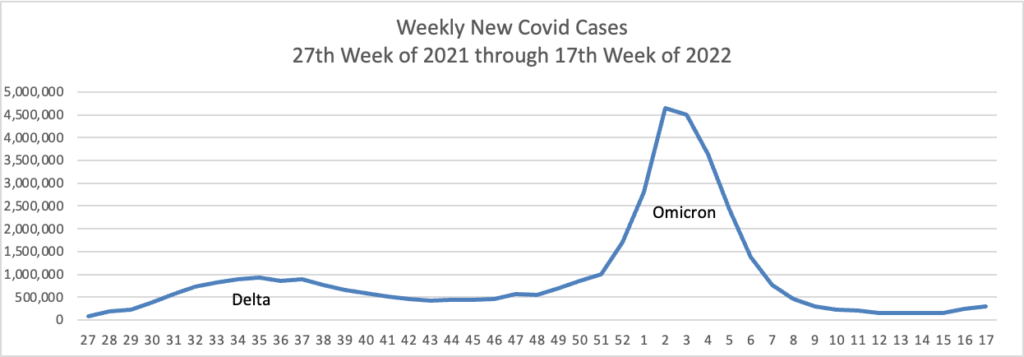
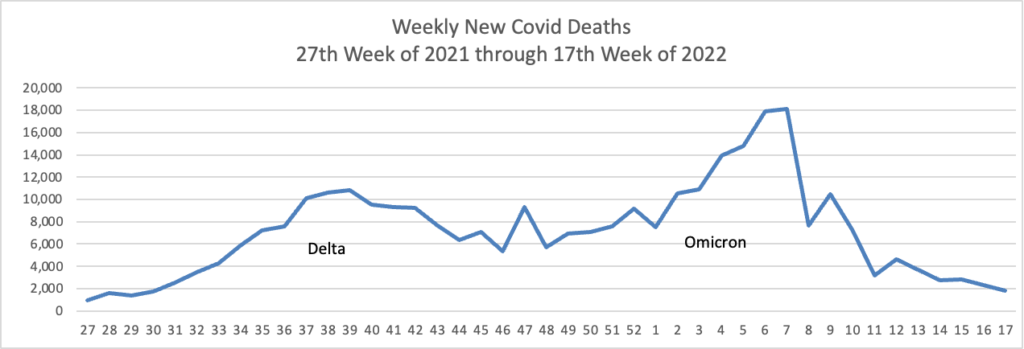
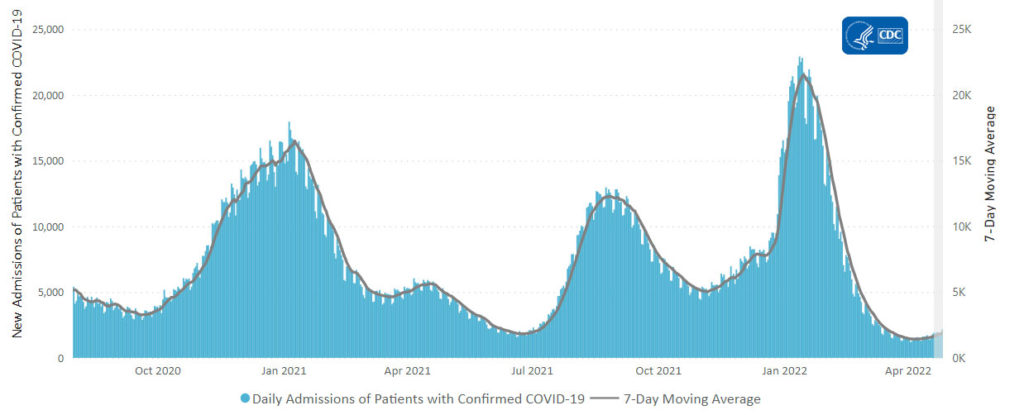
From the Omicron and siblings front
The Wall Street Journal informs us
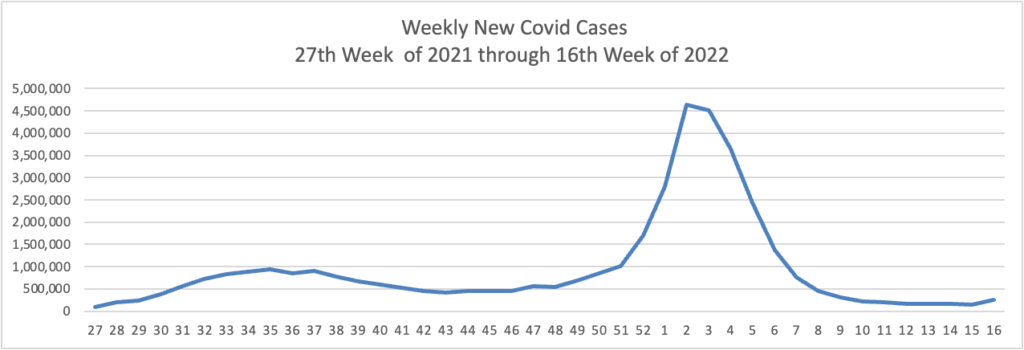
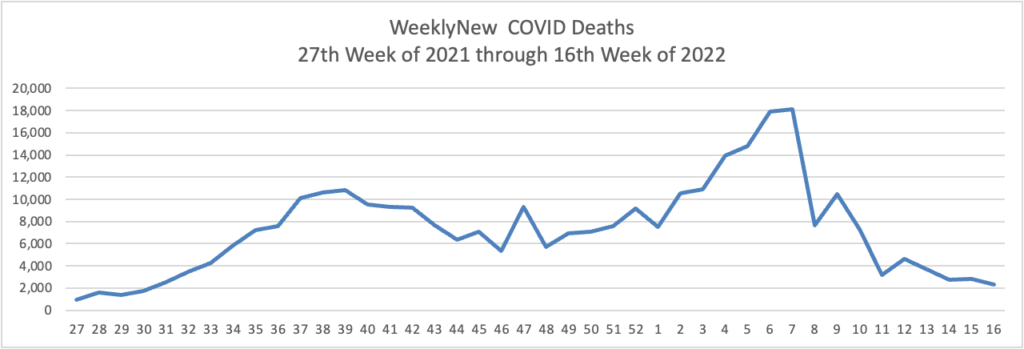
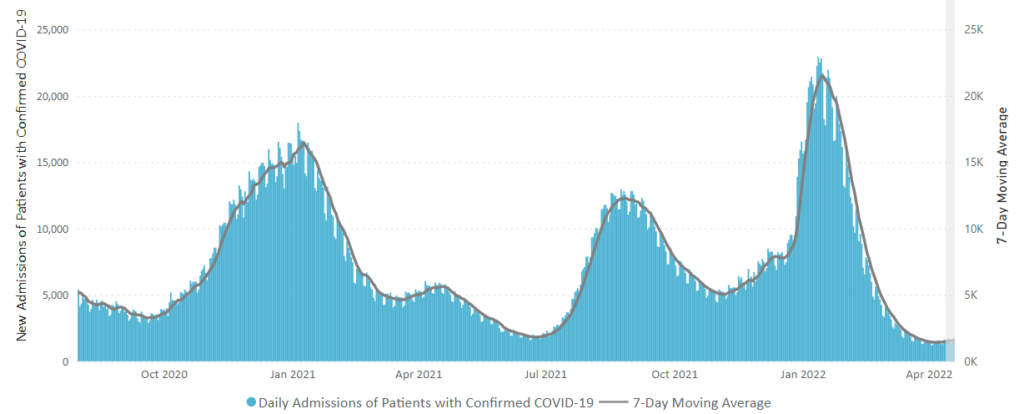
As new Omicron variants further infiltrate the U.S., a jumble of signals suggest the latest increase in Covid-19 infections hasn’t sparked a commensurate surge in severe illness even as risks remain.
Covid-19 virus levels detected in wastewater in the Northeast, the first region to see significant concentrations of the easily transmitted Omicron BA.2 variant, appear to have flattened out in the past two weeks. Covid-19 hospital admissions have risen in the region, but they remain far below levels during earlier surges that indicated widespread severe illness and taxed healthcare facilities.
“This wave of Covid in the United States, in the places where it is, is not dangerous in a way that prior waves of Covid were,” said Megan Ranney, an emergency physician and academic dean at Brown University’s School of Public Health.
The fast-mutating virus still poses risks, she said.
The new Fortune Well website offers timely guidance on the symptomatic differences between Covid and allergies.
Bloomberg Prognosis posted its late April Word Covid resilience rankings. Norway rides atop the rankings for the second month in a row The U.S. dropped six rankings to 30th. The article notes that the U.S. and the U.K are “weighed down by ongoing fatalities—their Covid Mortality Rate scores are among the worst of developed economies.
From the Affordable Care Act front, Health Affairs Forefront posted the ever-reliable Katie Keith’s first of three articles on the final 2023 ACA notice of benefit and payment parameters that was issued last week. This article’s section on Essential Health Benefits is relevant to FEHB carriers as each of them must select an EHB benchmark in order to apply the ACA’s restriction on annual dollar limits. The article’s section on Medical Loss Ratio is relevant to community-rated FEHB plans who generally use that benchmark to determine the reasonableness of their prices.
From the Rx coverage front, Medcity News reports “Bristol Myers Squibb drug Camzyos has received FDA approval for treating obstructive hypertrophic cardiomyopathy, a rare and potentially fatal heart disorder. The drug is projected to become a blockbuster seller, and its approval marks a payoff for BMS’s 2020 acquisition of the medicine’s developer, MyoKardia.”
From the telehealth front, mHealth Intelligence informs us
A majority of clinics (79 percent) used telemedicine to provide contraceptive services during the COVID-19 pandemic, according to a recent study published in the journal Reproductive Health.
For the study, researchers surveyed 907 US providers and clinic staff between April 10, 2020, and Jan. 29, 2021. They collected data on contraceptive service delivery challenges and strategies, including telehealth. The sample of respondents included physicians (17 percent), advanced practice clinicians (41 percent), registered nurses (16 percent), and health educators and social workers (11 percent).
The respondents practiced in a wide array of care settings, including youth clinics/school-based health centers or college health centers (36 percent), primary care clinics or health departments (29 percent), family planning clinics (22 percent), and independent abortion care clinics (4 percent). They saw, on average, 3,184 contraceptive patients annually.
Though only 11 percent of the clinics offered telemedicine for contraceptive services before the pandemic, this figure shot up to 79 percent after March 2020.