Midweek Update
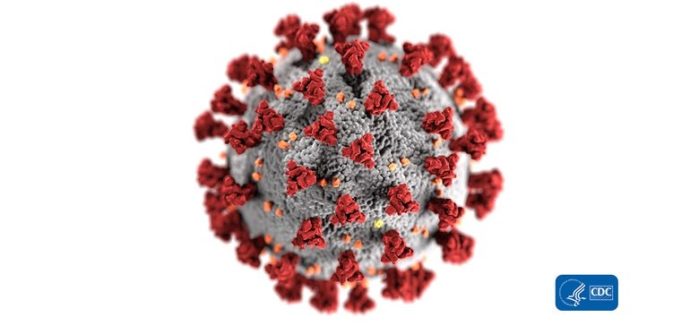
The Office of Personnel Management issued a guidance letter to FEHB carriers on the COVID-19 virus today.
The Internal Revenue Service today issued a Notice 2020-15 which permits high deductible health plans used with health savings accounts (under Internal Revenue Code Section 223) to cover COVID-19 testing on a first dollar basis. To its credit, OPM references the IRS notice in the above linked carrier letter.
The U.S. Labor Department also issued FAQ guidance on COVID-19 or Other Public Health Emergencies and the Family and Medical Leave Act.
As noted on Monday, this is Patient Safety Awareness week. The patient safety organization ECRI Institute released a list of top 10 patient safety concerns. The Safety Week’s key sponsor HHS’s Agency for Healthcare Quality and Research issued
Making Healthcare Safer III, a comprehensive report whose pages are filled with practical information on how today’s clinicians can keep patients free from harm.
The report reviews roughly four dozen practices that target patient safety improvement across a variety of settings. If appropriately applied, many of these practices can dramatically reduce high-impact healthcare-related harms.
The 47 patient safety practices and evidence highlighted in the report include technological and staffing-related practices, a series of specific hygiene and disinfection interventions for reducing healthcare-associated infections, and several practices designed to prevent medication errors and reduce opioid misuse and overdoses.