Thursday Miscellany
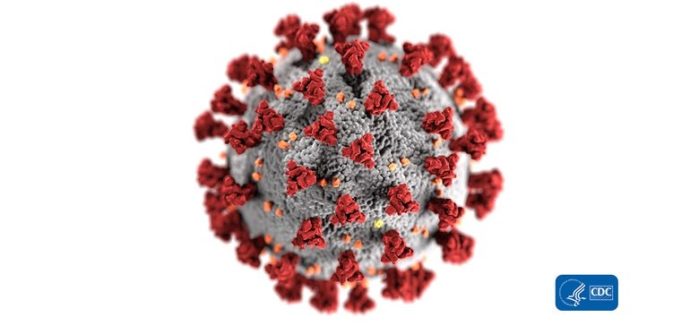
The Centers for Disease Control updated their guidance on how COVID-19 spreads earlier this week. Here’s the main takeaways from the FEHBlog’s standpoint:
COVID-19 is thought to spread mainly through close contact from person-to-person. * * * Some people without symptoms may be able to spread the virus. The virus that causes COVID-19 is spreading very easily and sustainably between people. Information from the ongoing COVID-19 pandemic suggests that this virus is spreading more efficiently than influenza, but not as efficiently as measles, which is highly contagious. In general, the more closely a person interacts with others and the longer that interaction, the higher the risk of COVID-19 spread.
Check it out.
Healthcare Dive reports
The Trump administration on Wednesday proposed changes to how drugmakers can report their prices to Medicaid, seeking to make it easier for pharmaceutical companies and insurers to enter into contracts that tie payment to patient outcomes. Typically, drug contracts are linked to the volume of product sold, providing for larger manufacturer rebates the more a product is prescribed and covered by an insurer. Increasingly, however, drugmakers and insurers have been exploring alternative approaches centered on some measure of a medicine’s value.
Why is this relevant to the FEHBP? “The Medicaid best price policy requires drug manufacturers to give Medicaid programs the best price among nearly all purchasers [Medicare Part D is excepted].” So for example, if a prescription drug manufacturer cuts a deal for value based drug pricing, the VBD pricing cannot drop below the Medicaid price. If the manufacturer can cut the same deal with Medicaid under this proposed rule, then everyone benefits. This is a proposed rule that won’t go into effect until later this year at best.
Fierce Healthcare reports that
Health Care Service Corp., which owns and operates Blue Cross plans in five states, has tapped Epic to develop a data exchange platform between health plans and providers. HCSC health plans will be able to exchange medical information with health providers in its networks that use Epic’s electronic health record (EHR) software. The contract is one of the first of its kind between Epic and a large insurer, according to the companies.
Given the importance of clinical data in government and large employer healthcare quality programs imposed on health plans, including OPM’s Plan Performance Assessment, this certainly won’t be the last such deal.