Monday Roundup

The President has declared May 1 through May 7 to be Public Service Recognition Week. OPM explains
Celebrated annually during the first week of May since 1985, Public Service Recognition Week (PSRW) (external link) is time set aside to honor the men and women who serve our nation as federal, state, county and local government employees.
Throughout the country, mayors, governors, agency leaders, communities and public service organizations participate in PSRW by issuing proclamations; hosting award ceremonies and special tribute events; and delivering messages about the value of public service.
To that end, Govexec reports the President took the time today to virtually award Presidential Rank Awards to 230 senior federal employees from 37 agencies.
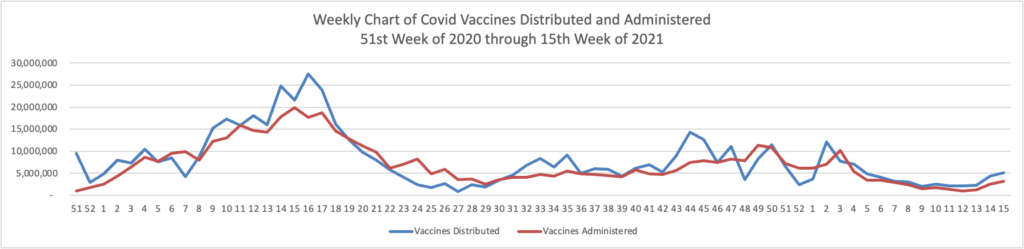
Speaking directly to the career civil service, Biden said: “Over the last 15 months you’ve helped us deliver so much to the American people,” such as the getting Americans vaccinated against COVID-19, delivering economic relief checks, caring for veterans, implementing the infrastructure package and working to restore the public’s faith in government and democracy. He gave a big “thank you” to them as well as their families.
The FEHBlog heartily agrees.
From the Omicron and siblings front, WebMd informs us
The FDA’s independent panel of advisors will meet in June to discuss the Pfizer and Moderna COVID-19 vaccines for children under age 5, as well as the Novavax vaccine for adults, according to an FDA announcement released Friday.
On June 7, the FDA’s vaccine committee will review the Novavax shot, which could become the first new COVID-19 vaccine to hit the U.S. market in more than a year. The shot is already authorized in more than three dozen countries, including across Europe.
The FDA has also selected three possible dates — June 8, 21, and 22 — to discuss the shots for kids under age 5. The dates are tentative because the companies haven’t completed their submissions, the agency said.
The FEHBlog is pleased to read about these developments because the Novovax shot which uses a traditional vaccination approach may be acceptable to the vaccine inquisitive and the country needs a vaccine for younger children.
STAT News adds
Pfizer released news late Friday that Paxlovid, the antiviral currently subject to a big push from the U.S. government, failed to prevent people living with Covid patients from catching the infection.
The news is one of several bad headlines for the new Covid pill, but one experts say doesn’t affect the medicine’s primary use: treating people who are already sick.
Paul Sax, clinical director of the division of infectious diseases at Brigham and Women’s Hospital, said he would “absolutely” prescribe Paxlovid to people at high risk of severe disease who have Covid. “Without hesitation,” he said. “Because the net benefit in the high risk study was extremely high.”
From the Affordable Care Act front, Health Affairs Forefront has posted the second part of Katie Keith’s three-part series on last week’s HHS final 2023 notice of ACA benefit and payment parameters. The second part concerns changes specific to the ACA marketplace or exchange plans.
From the Rx coverage front, Health Affairs informs us
UnitedHealthcare is restricting insurance coverage of Aduhelm across all of its health plans, saying the drug “is unproven and not medically necessary for the treatment of Alzheimer’s disease due to insufficient evidence of efficacy,” according to the company’s new policies.
Physicians who plan on giving Aduhelm to UnitedHealthcare patients will need to obtain prior approval from the insurance company, effective June 1. Patients also need to be in an approved clinical trial.
UnitedHealthcare’s decision follows Medicare, which said last month it would only pay for the costly infusion drug for patients who participate in a clinical trial. UnitedHealthcare is the largest Medicare Advantage insurer in the country, covering 8 million people older than 65 and people with disabilities, making this policy particularly important for older Americans on those private plans.
The FEHBlog expects UHC’s announcement to be the tip of the eventual iceberg of similar Aduhelm coverage decisions.
Following up on previous stories mentioned in the FEHBlog, the Wall Street Journal reports
Online pharmacy company Truepill Inc. said it is temporarily halting prescriptions for Adderall and other controlled substances used to treat attention-deficit hyperactivity disorder, and partner Cerebral Inc. told its clinicians to direct those orders to patients’ local pharmacies.
Cerebral, an online mental-health company based in San Francisco that describes Truepill as its preferred pharmacy, informed its clinicians of Truepill’s decision in a Friday email viewed by The Wall Street Journal. The email said Truepill would no longer support mailing Schedule 2 controlled substances, including Adderall and Vyvanse, “to any of their customers.”
Truepill said that, “out of an abundance of caution,” it is temporarily pausing all fulfillment of Schedule 2 substances while it evaluates appropriate next steps. It said Schedule 2 substances such as Adderall make up less than 1% of its total prescription volume. Truepill didn’t provide a list of other partners affected by its decision.
Some of the nation’s largest pharmacies have blocked or delayed prescriptions over the past year from clinicians working for telehealth startups that have sprung up to treat ADHD, according to pharmacies and people familiar with the issue.
The Journal reported last week that pharmacies including Walmart Inc., CVS Health Corp. and Walgreens Boots Alliance Inc. have blocked or delayed prescriptions for companies treating ADHD online or have blocked individual prescribers, according to people familiar with the issue.
That was the right outcome as far as the FEHBlog is concerned.
In U.S. Supreme Court news, Business Insurance reports “Private plaintiffs cannot be reimbursed for emotional distress damages under the 1973 Rehabilitation Act and the Patient Protection and Affordable Care Act, the U.S. Supreme Court ruled” last Thursday in the linked opinion. The Affordable Care Act provision at issue is the ACA’s convoluted individual non-discrimination provision, Section 1557.
From the healthcare business front, Fierce Healthcare tells us
Outpatient volumes and revenue for hospitals and health systems showed a robust rebound in March as expenses eased due to fewer extremely sick patients, a new report said.
Consulting firm Kaufman Hall released its latest hospital flash report Monday (PDF) detailing the impact of system finances for the month of March. A key takeaway from the report is that while actual hospital margins were negative for the third month in a row, outpatient revenues had a massive bump.
“While the road to recovery remains long for many hospitals, these trends indicate some pressures of the pandemic may be lifting,” said Erik Swanson, senior vice president of data and analytics with Kaufman Hall, in a statement.
From the mental healthcare front,
Fierce Healthcare reports
Mental health concerns are on the rise across the board, and especially among Blacks, seniors, young adults and LGBTQIA people, a new survey finds.
CVS Health and Morning Consult polled more than 2,200 adults in early April and found that 59% of respondents have experienced challenges with their mental health or that of a friend or family member. That is a 9% increase over 2020 survey data.
More than half (57%) of people surveyed who identify as LGBTQIA expressed concern about their own mental health, 20 percentage points higher than other groups included in the study. Nearly three-quarters (74%) of those aged 18 to 34 said they experienced such concerns either themselves or for a friend or family member, up 12 percentage points from 2020.
The survey also found an 11 percentage point increase in mental health concerns among Black respondents compared to pre-COVID levels. A double-digit increase was also found among people over age 65; about 40% reported mental health concerns for themselves or family and friends, up 10 percentage points from 2020.
AHIP describes ten ways that people can get the mental healthcare services that they need.