Thursday Miscellany
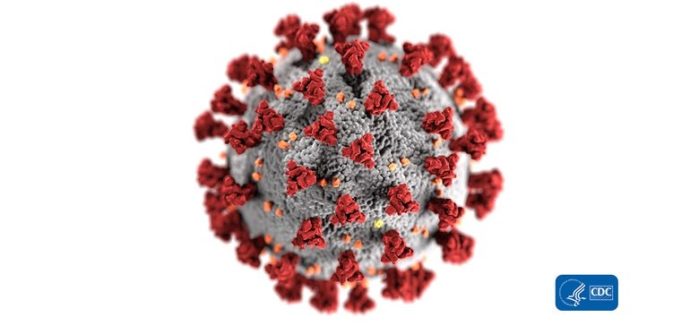
Regrettably, the Wall Street Journal reported today a spike in COVID-19 cases in States, like Texas, Utah, Arizona, and Arkansas, that were not hard hit early on in the COVID-19 emergency.
Experts analyzing states with worrisome trends in serious cases are largely pointing to the onset of summer, when people began to congregate in resort spots. [FEHBlog note: Super-speader events are risky.]
Some also suspect that officials who allowed businesses to reopen after a relatively calm few weeks might have sent an inadvertent message that the problem had largely passed.
As if responding to the suspicious “some,” the Centers for Disease Control has released a social media toolkit to spread COVID-19 related advice on Facebook, Instagram, Twitter etc.
It’s worth noting that the Wall Street Journal editorial page’s observation that “More infections are inevitable as states reopen, and there will be much trial and error. States need to be vigilant for outbreaks and protect high-risk areas and the vulnerable. But the costs of shutting down the economy are so great, in damage to lives and livelihoods, that there is no alternative to opening for the broader public good.”
In other news —
- Healthcare IT News reports that
A new study published in the Journal of the American Medical Association found that one-fifth of patients who read ambulatory care notes reported finding a mistake in those notes, and 40% of those regarded the error as serious.
“Among patient-reported very serious errors, the most common characterizations were mistakes in diagnoses, medical history, medications, physical examination, test results, notes on the wrong patient, and sidedness,” the study authors explained.
That’s worrisome for patient healthcare as well as for other doctors and health plans who rely on these reports.
- Health Payer Intelligence offers a thought provoking article on four data points that illustrate mental health parity. The rub is that “Mental and behavioral healthcare parity is about more than just equal reimbursement with similar medical and surgical services. It includes ensuring access to care by having enough providers in-network and making sure that the right types of specialists are available for members.”