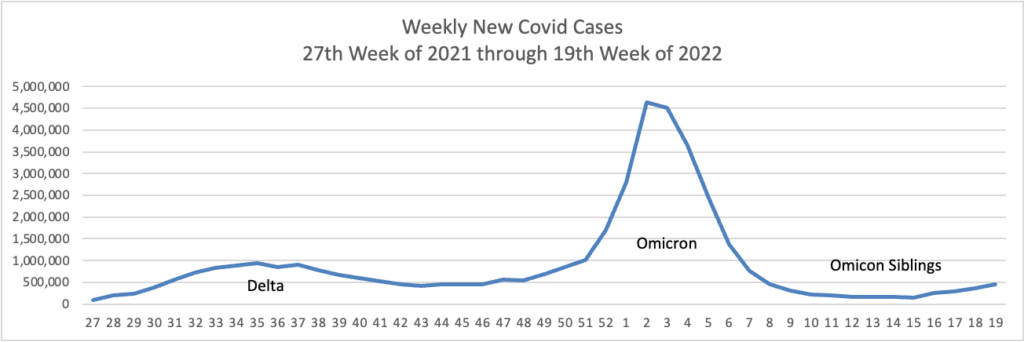
Based on the CDC’s Covid Data Tracker and using Thursday as the first day of the week, here is the FEHBlog’s weekly chart of new Covid cases from the 27th week of 2021 through the 19th week of 2022.
The CDC’s weekly review of its Covid statistics notes
As of May 11, 2022, the current 7-day moving average of daily new cases (84,778) increased 30.7% compared with the previous 7-day moving average (64,863). A total of 82,087,117 COVID-19 cases have been reported in the United States as of May 11, 2022.
Here’s the CDC’s weekly chart of new Covid hospitalizations
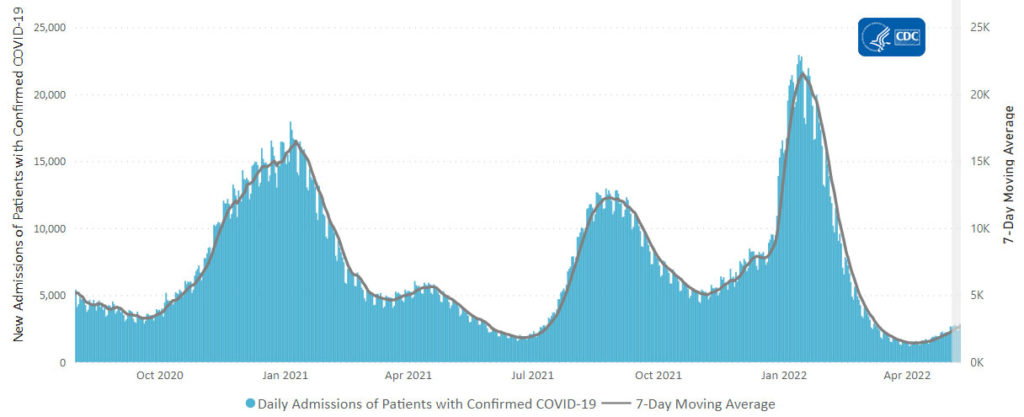
The CDC’s weekly review of Covid hospitalization notes, “The current 7-day daily average for May 4–10, 2022, was 2,629. This is a 17.5% increase from the prior 7-day average (2,238) from April 27–May 3, 2022.”
Here’s the FEHBlog’s weekly chart of new Covid deaths from the 27th week of 2021 through the 19th week of 2022:
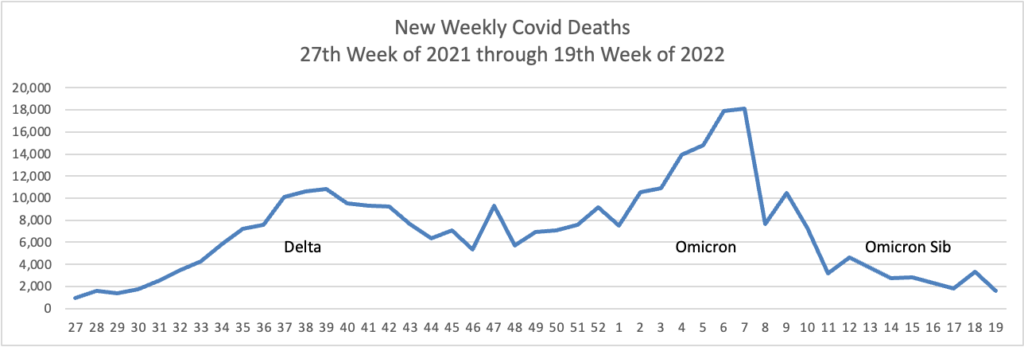
The CDC’s weekly review notes “The current 7-day moving average of new deaths (273) has decreased 15.4% compared with the previous 7-day moving average (322). As of May 11, 2022, 996,376 COVID-19 deaths have been reported in the United States.”
Finally, here is the FEHBlog’s weekly chart of Covid vaccinations distributed and administered from the beginning of the Covid vaccination era through the 19th week of 2022.
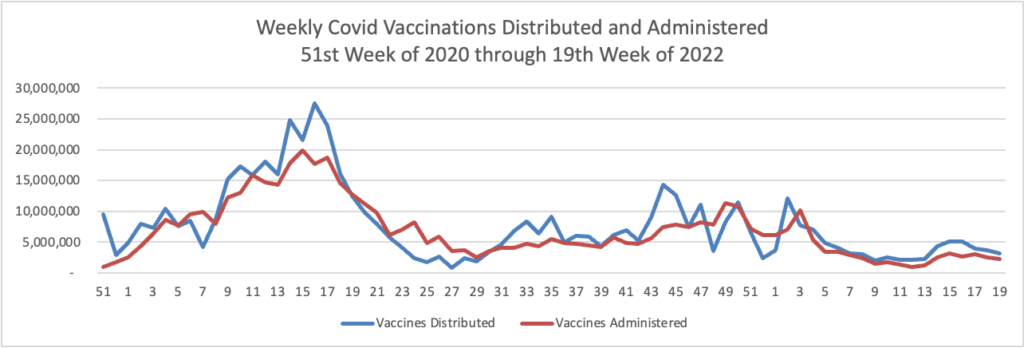
Per the CDC’s weekly review, “As of May 11, 2022, the 7-day average number of administered vaccine doses reported (by date of CDC report) to CDC per day was 390,306, an 11.1% decrease from the previous week.”
76% of the U.S. population aged 18 and older are fully vaccinated against Covid, and 50% of that cadre has received the first booster. Likewise, 90% of the U.S. population aged 65 and older is fully vaccinated, and 70% of that cadre has received the first booster. There is work still to be done but the public health community and the U.S citizenry deserves credit for these accomplishments.
To wrap up this week’s Covid stats, let’s include the CDC’s latest Communities report:
As of May 12, 2022, there are 137 (4.25%) counties, districts, or territories with a high COVID-19 Community Level, 453 (14.07%) counties with a medium Community Level, and 2,630 (81.68%) counties with a low Community Level. This represents a small (+1.77 percentage points) increase in the number of high-level counties, a moderate (+4.10 percentage points) increase in the number of medium-level counties, and a corresponding (−5.87 percentage points) decrease in the number of low-level counties. Eight (15.38%) of 52 jurisdictions had no high- or medium-level counties this week.
To check your COVID-19 Community Level, visit COVID Data Tracker.
NPR Shots offers a valuable article describing three ways to get the Paxlovid pill if diagnosed with Covid. The key takeaway from the FEHBlog’s perspective is the need to have a primary care provider in your life.
For those with health insurance and access to their primary care providers or health care team, you can make an in-person or telehealth appointment to get tested (or share your positive test results), assessed for risks and medications and, if eligible, obtain a prescription for the pills.
You’d then get the prescription filled at a nearby pharmacy.
Having a provider that knows your medical history, as well as the details of your current situation, can be very helpful, says Dr. Ulrika Wigert, a family medicine physician at CentraCare in Sauk Center, Minnesota. “Did you test the first day [of symptoms]? Did you test the second day? How sick were you when you tested?” And, if you’re starting to feel better by the time you get the medication, do the benefits of taking the medication outweigh any risks? “Having a provider help navigate that on the individual patient basis” can help guide you through an appropriate course of care, she says.
STAT News addresses three burning questions about the future of prescribing drugs using telehealth services (not for a PCP visit).
Research by Lori Uscher-Pines, a senior policy researcher at RAND, suggests that providers are starting to prescribe buprenorphine — a controlled substance used to treat opioid use disorder — without in-person visits. But they’re typically more comfortable continuing the prescriptions virtually for patients they’ve already met, compared to taking on new patients virtually.
Still, “very few studies of medication treatment for opioid use disorder via telehealth have shown safety or diversion concerns,” she said. And she noted that one recent study suggested that relaxed restrictions have improved treatment retention for opioid use disorder patients.
Telehealth prescription could help patients in regions with acute clinician shortages — especially of mental health providers — obtain critical medication.
“A key question going forward is how to strike a balance between increasing access to important medications on the one hand and limiting the potential for misuse on the other,” Uscher-Pines said.
In the past, federal and state regulations have required clinicians to frequently examine patients in-person to guard against misuse, addiction, or fraud. “But are there other ways to accomplish this, perhaps ways that actually leverage telehealth rather than restrict it?” she asked.
A better system might involve hybrid care: In-person exams for certain types of prescriptions blended with virtual follow-ups, for instance. But Schwamm cautioned against over-regulating telehealth prescriptions, given that clinical guidelines evolve faster than federal and state policies typically do.
“Whenever you put these kinds of restrictions in place, you are restricting access to care,” he said. “Do we need to require, and is it good medical practice, to require by regulation that the person come in-person? I would argue that we just don’t know.”
It’s complicated.
